What is Burkitt’s Lymphoma
Page Contents
- 1 What is Burkitt’s Lymphoma
- 2 What Causes Burkitt’s Lymphoma
- 3 What are the Types of Burkitt’s Lymphoma
- 4 Signs and Symptoms
- 5 Complications
- 6 Diagnosis and Tests
- 7 Treatment and Management
- 8 Prognosis and Survival Rates
- 9 BL Prevention
- 10 Incidence and Prevalence
- 11 Burkitt’s lymphoma ICD‑9‑CM and ICD‑10 Codes
Burkitt’s lymphoma (BL), also called Burkitt lymphoma, Burkitt’s tumor, or malignant lymphoma, is a rare cancer of the lymphatic system, particularly of the B cells, accounting for about 0.3% to 1.3% of all non-Hodgkin lymphomas. The condition is named after British surgeon Denis Burkitt, who discovered the disease in African children and young adults. Considered to be the fastest growing tumors affecting humans, it may spread to various parts of the body.
What Causes Burkitt’s Lymphoma
Impaired Immunity: It is often associated with a weak immune system, with the condition often detected in African children suffering from Malaria. It is believed that BL occurs when malaria weakens the immune system’s reaction towards the Epstein-Barr virus (responsible for nasopharyngeal lymphoma, glandular fever and mononucleosis), such that the infected B cells are converted to cancerous cells. The mode of transmission of EBV is usually through saliva.
Genetic Factors: It may have some other causative factors apart from an impaired immune system, like chromosomal translocation involving chromosome 8, which may alter the mode of expression of the gene, c‑Myc, thereby disrupting its normal function. This can lead to an unrestrained growth of B lymphocytes, resulting in the cancerous disorder.
What are the Types of Burkitt’s Lymphoma
The condition can be classified into three types:
- Endemic (African): Always associated with chronic malaria and EBV infection, it can affect the gastrointestinal tract, ovaries, breasts and central nervous system.
- Sporadic (Non African): May or may not be associated with EBV infection, and often involves the liver, colon spleen, bone marrow, brain or spinal fluid.
- Immunodeficiency Related: Usually associated with the intake of immunosuppressive drugs, such as those used for preventing organ transplant rejection or treating HIV and AIDS.
Risk Factors: Who is Likely to Have BL
- Young boys between 5 and 8 years of age
- Although rare in adults, males are more at risk
- People with a weak immune system like those infected with HIV/AIDS
- Those living in regions of North Africa, South America, the Middle East and Papua New Guinea
Signs and Symptoms
Common Symptoms
- Fever
- Loss of weight
- Night sweats
- Distortion of bones of the face
- Loss of appetite
Endemic BL
A swollen lymph node is one of the earliest symptoms of this type of BL. Swelling of lymph nodes in the chest or neck may lead to:
- Sore throat
- Swallowing difficulty
Another endemic symptom involving the oral cavity comprises of fast growing tumors of the jaw (mandible), or some other facial bone that have a doubling time of 24 hours. It mostly occurs in children.
Sporadic and Immunodeficiency Related BL
- Pain in the abdomen
- Feeling of a heavy, abdominal mass
- Enlarged tonsils
The condition may spread to other body parts, leading to characteristic symptoms.
Related to the GI Tract
- Diarrhea
- Nausea
Related to the Central Nervous System
- Headache
- Seizures
- Mental confusion
- Paralysis
Related to the Bone Marrow
- Shortness of breath and weakness suggesting anemia
- Bleeding from bowel or any other bruise indicating low platelet count
Complications
- Intestinal obstruction
- Tumour lysis syndrome
- Peripheral neuropathy
- Leukaemic transformation
Diagnosis and Tests
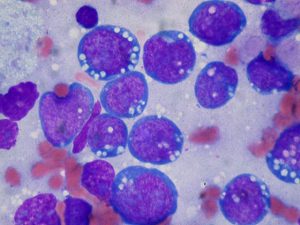
Since the symptoms have a sudden onset, early diagnosis is required. After a physical examination, a biopsy of all or a portion of a swelled lymph node or other suspicious regions is done to confirm the disease. A microscopic view of the affected tissue reveals a “starry sky” appearance, typical of the condition.
http://www.ganfyd.org/images/9/93/Burkitt_lymphoma_starry_sky_1.jpg
Burkitt’s Lymphoma Starry Sky Appearance
Other relevant tests may involve:
- Computed tomographic (CT) imaging of certain body parts such as the chest, pelvis, abdomen to find out the concerned lymph nodes and organs
- Examination of bone marrow and spinal fluid
- X-ray of the chest
- MRI scan or PET scan
- An ECG or MUGA scan to check if the heart is working properly or not
- A 24-hour urine collection to determine kidney function
- Blood tests to find out liver function
- Tests to detect HIV infection
- Peripheral blood smear
Differential Diagnosis
- Lymphoblastic lymphoma
- Blastic mantle cell lymphoma
- Diffuse large B-cell lymphoma
- Prolymphocytic SLL/CLL
BL Staging
Different stages of the condition that depend on the location and nature of the swollen lymph nodes as well as organ involvements are:
Stage 1: Lymphoma occurring either above or below the diaphragm, but is restricted to a single group of lymph nodes only
Stage 2: Lymphoma occurring in either two or more locations on the same side of the diaphragm
Stage 3: Lymphoma occurring on both sides of the diaphragm
Stage 4: Lymphoma found in bone marrow or central nervous system
Treatment and Management
Intensive Intravenous Chemotherapy
This is often the preferred treatment with a high success rate since it may successfully destroy most of the lymphoma cells.
Intrathecal Chemotherapy
Also called CNS prophylaxis, this is carried out by injecting the chemotherapy drugs directly into the spinal fluid, since the condition may spread to the fluid that surrounds the brain and spinal cord. The drugs that are used in various combinations include cyclophosphamide (Cytoxan), doxorubicin (Adriamycin), cytarabine (Cytosar-U, Tarabine PFS), and methotrexate (Rheumatrex).
Intrathecal chemotherapy is at times used in combination with other treatments such as:
- Treatment with a monoclonal antibody called, rituximab (Rituxan), which gets attached to a protein CD20 present on the surface of cancerous B cells, that stimulates the immune system to destroy the damaged cells.
- Transplantation of stem cells, carried out by removing, storing and returning stem cells to the body of the diseased individual
- Radiation therapy
- Steroid therapy
Surgery
In the case of intestinal obstruction, surgery is carried out.
New Treatments for BL
According to the findings of a new clinical trial, treatment with low-intensity chemotherapy may increase the survival rate of adult patients having BL.
Treatment of Associated Conditions
- Mesna and folinic acid to help combat the side effects induced by the chemotherapy drugs
- Administration of rasburicase (Fasturtec) initially, and later allopurinol (Zyloprim) to provide protection against tumor lysis syndrome
- Anti-sickness drugs (antiemetics)
- Prophylactic (preventive) antibiotics and antifungals, to reduce infection risks
- Growth factors (G-CSF), so that there is a fast recovery of the bone marrow
Follow-up Treatment
A patient is required to have monthly checkups after chemotherapy to detect if the lymphoma is relapsing or not. The rate of such checkups is decreased, if, at the end of six months, lymphoma does not recur. However, there can be long term side effects like reduced fertility and heart ailments.
Prognosis and Survival Rates
The outcome generally depends on the stage of BL at the time of diagnosis as well as the age of the patient. If the cancer has not spread, the survival rate is as high as 90% for both adults and children. However, the outlook for elderly patients is usually poor. The condition rarely occurs during pregnancy, but has a poor outcome when it does.
BL Prevention
Though there are no known ways to prevent BL, certain lifestyle modifications such as reducing HIV infection risks in relation to the sporadic form, may aid in reducing the possibility of having the disease. The condition may also be handled naturally by maintaining a healthy diet consisting of sprouts, and green vegetables.
Incidence and Prevalence
Sporadic BL is rare in developed countries; about 1200 people in the US are diagnosed with the condition each year. Endemic BL, on the other hand, has a high incidence in Africa, accounting for about one-half of childhood cancers.
Burkitt’s lymphoma ICD‑9‑CM and ICD‑10 Codes
The ICD‑9‑CM code of Burkitt’s lymphoma is 200.2, and the ICD‑10 code is C83.7.