The post Ulcerative Colitis | Pictures, Causes, Symptoms, Diagnosis, & Treatments appeared first on Prime Health Channel.
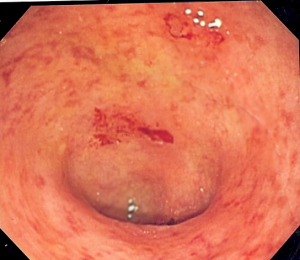
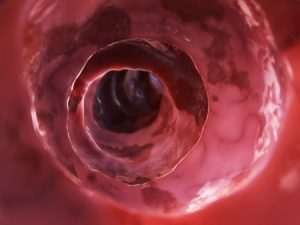
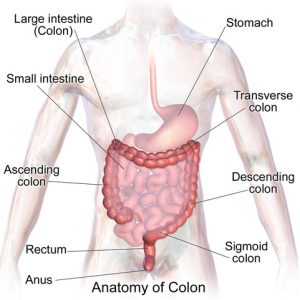
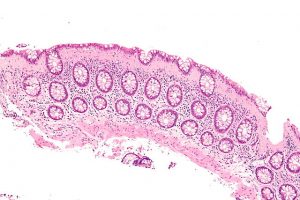
]]>Ulcerative Colitis is a bowel disease that affects the colon or large intestine. It is also known as IBD (Inflammatory Bowel Disease) and incorporates a set of diseases affecting the gastrointestinal tract. It develops when the large intestine and rectum get inflamed resulting in tiny sores or ulcers on the colon lining. It starts in the rectum and spreads upwards involving the entire colon.
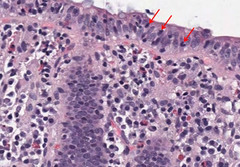
Inflammation induces bowel to move rapidly and discharge its contents quickly. Bowel lining has surface cells which die to form ulcers that release pus, mucus and also bleeding. It affects all ages, but mostly people between 15-35 age groups are diagnosed. UC have similar symptoms like irritable bowel syndrome and Crohn’s disease.
Difference between Ulcerative Colitis and Crohn’s disease
- Ulcerative Colitis: UC is limited to rectum and colon. It is a continuous pattern with intestine lining and inflammation. Patients can experience a relapse next year.
- Crohn’s disease: It can develop everywhere in GI tract between mouth and anus. It appears in patches that might extend through the thickness of the bowel wall. Patients will have minimum one relapse in next five years.
Causes
UC is a result of immune system failing to defend a bacteria or virus from inflaming intestinal walls. Other reasons are:
- Genetic: Risk increases if UC is prevalent in family history.
- Environmental Toxins: Single factor is not responsible for IBD and experts have detected viruses from tissue samples of patients.
- Psychological Factors: Stress might modify or worsen the disease.
- Immune System: Several changes contribute to the cause of IBD.
Symptoms
- Proctosigmoiditis: Inflammation in the sigmoid colon (lower end) and rectum along with abdominal cramps and pain, bloody diarrhea, urgency, rectal bleeding, etc.
- Ulcerative proctitis: Irritation only in the rectum with rectal bleeding. In severe conditions, rectal pains with a sudden urge to defecate, the panic of soiling, and painful bowel movement.
- Acute severe ulcerative colitis: Affects entire colon with profuse diarrhea, severe pain, fever, bleeding, etc.
- Left-sided colitis: Irritation expands from sigmoid to the rectum with signs like abdominal pain, weight loss, and bloody diarrhea.
- Pancolitis: Affecting the entire colon (left, right, transverse colon and rectum), it has rounds of severe bloody diarrhea, abdominal pain, weight loss, night sweats and fatigue.
- Fulminant Colitis: Rare and chronic type of pancolitis with severe dehydration, bloody diarrhea, abdominal cramps, and Patients can develop toxic megacolon and perforation (colon rupture).
Other Symptoms
- Soreness or Joint pain
- Anemia
- Appetite loss
- Sudden urge to go (especially at night)
- Feeling full (full colon) after using the bathroom
- Unable to hold stool
Symptoms get worse in the morning. However, it depends upon the bowel part affected.
Risk Factors
- Age: Usually seen before the age of 30, it affects men and women both.
- Race: It can occur in any race (specifically to the Ashkenazi Jewish descent, from Russia and Europe)
- Family History
- Accutane (Isotretinoin): Although it treats acne, it has been found to be the underlying cause.
Complications
- Bone loss
- Inflammation in eyes, joints and skin
- Colon cancer (Starts after 9-10 years of UC)
- Severe Bleeding (intestinal)
- Dehydration
- Perforated Colon
- Colon Swelling
- Liver disease
- Intestinal wall thickening
- Blood infection
- Kidney stones
- Blood clots in arteries and veins
- Erythema Nodosum (Painful red skin)
- Uveitis (Painful red eyes, also risk permanent vision loss)
Diagnosis
UC is confused with other diseases due to similar symptoms and multiple tests will help experts to diagnose. The tests include:
- Endoscopy: Flexible tube is used to examine small intestine, esophagus and
- Stool test: Stool is examined for parasites, blood, and
- Biopsy: Tissue sample is removed for examination from the colon and it allows knowing the intensity.
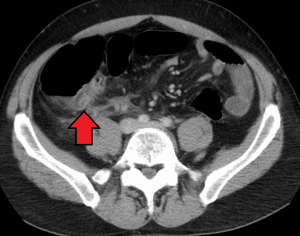
- CT scan: Particular X-ray for pelvis and abdomen
- Colonoscopy: Flexible tube is inserted to examine the rectum and visualize intestine. Colonoscopy allows direct visualization of the extension of colitis. Small tissues are also received during the process to check the severity.
- Blood tests: Complete blood count helps in detecting anemia, high sedimentation rate, C-reactive protein, kidney function, liver function, etc.
- Calprotectin: Responsive marker of the disease, it elevates before severe symptoms arise suggesting IBD. However, a single test cannot determine the condition.
- X-Ray: During the process, the liquid chalky substance is inserted into the rectum to inject the colon. Barium is dense and does not allow X-ray to pass through. Hence the outline is visible on X-ray images. However, it is inferiorly accurate than colonoscopy and direct visualization. If barium enema (X-ray) is done and UC is assumed, colonoscopy is essential for further diagnosis.
Treatments
- Diet Changes: Food is not a cause but can worsen the situation. It is advisable to eat snacks and meals that are high in protein and calorie, but low in fiber.
- Medicine: Antibiotics will help to fight infections and heal. Aminosalicylates lowers inflammation and reduces the symptoms. In most chronic cases corticosteroid is prescribed. For chronic ulcerative colitis, biologics drugs (made from living cells) are used.
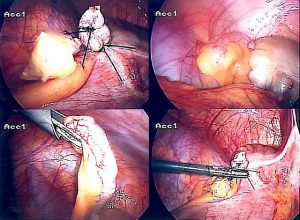
- Surgery: Only used if other treatments don’t work. It involves the removal of the rectum and entire colon, operation eliminates the chances of developing cancer. However, surgery is not for all, and it is reserved for some specific patients who are not responding to medications and have toxic megacolon. Patients with high risk of developing colon cancers or are suffering from colitis for a more extended period have reacted poorly to medicines.
In a standard surgery entire colon is removed and a small opening is left open at the end of the small intestine that forms ileostomy. Stool gets collected in the bag attached to the ileostomy. With recent improvements continent ileostomy is created from intestine that acts like a rectum and it is emptied regularly with a tube.
Pictures
Preventions
There is no evidence of what causes ulcerative colitis, but certain foods can worsen the situation. The following can help in preventing the disease to worsen:
- Minimize milk intake
- Avoid fatty foods
- Limit fiber-rich foods
- Eat small meals throughout the day
- Drink small amount of water throughout the day
- Avoid sodas (it will increase gas)
The post Ulcerative Colitis | Pictures, Causes, Symptoms, Diagnosis, & Treatments appeared first on Prime Health Channel.
]]>The post Right Side Abdominal Pain | Causes, Symptoms, Diagnosis & Treatments appeared first on Prime Health Channel.
]]>Cause of concern
The lower right part of the abdomen comprises of different organs like a colon (in case of men) and right ovary (in case of women). Many reasons can cause mild to serve pain in this area. In most cases, the pain which arises in the right lower abdomen is not a major concern as it may fade away on its own in a day or two. However, if the pain remains constant for few days, then it is recommended to go through a detailed check-up
Causes of Right Side Abdominal Pain
Appendicitis
The appendix is a thin and small tube located at the intersection of the small and large intestine. An inflamed appendix is defined as appendicitis and is supposed to be the most common cause.
Symptoms of appendicitis
- Nausea
- Vomiting
- Diarrhea
- Constipation
- Fever
- Swelling in abdominal
- Low appetite
Appendicitis is a serious condition wherein the doctors often recommend removal of the appendix through surgery. If left untreated, the appendix may rupture over time and cause other complications.
Other Common Causes
There are several other causes of pain on either side of the lower abdomen. It may also happen that the discomfort is experienced on the right side, but the cause of pain is on the left side. Some of the other causes have been listed below:
- Gas: The entire digestive tract is filled with intestinal gas formed by the food particles which are broken down completely until the time it reaches the colon. More the particles of undigested food left inside more are the gas produced. The stomach thus gives bloated or knotted feel in the stomach as more gas gets formed. The temporary relief of gas is burping and farting. But excessive gas is a sign of digestive disorder such as lactose intolerance and diabetes.
- Indigestion: Indigestion occurs after eating or drinking and may be a reason for the pain in the upper abdomen, but it may be felt in the lower abdomen. Although, slight indigestion fades away pretty quickly if the symptoms remain it can be concerning.
- Hernia: When an internal organ pushes out through a tissue or muscle which holds it in place, it is known as a hernia. Different types of a hernia may happen in the abdominal region.
- Kidney infection: Bacteria inside the bladder, uterus or urethra cause kidney infection that may affect both the kidneys causing the infection. The pain may be felt in the lower abdomen due to discomfort from the kidney infection. If this infection is not treated on time, it may cause permanent damage to the kidneys.
- Kidney stones: Salts and minerals build up to form a hard substance known as a kidney It eventually causes pain when it starts to move around or pass into the tube connecting the kidney and the bladder. The pain severely hits in the back and sides below the ribs and all over the lower abdomen and groin. The intensity of the pain depends on the movement of the kidney stone as it shifts and moves through the urinary tract.
- Irritable bowel syndrome: Irritable bowel syndrome (IBS) mostly affects the large intestines and is a chronic disorder. Although no conclusive evidence is found, doctors believe that the factors causing the syndrome are contractions that are stronger than the normal ones and abnormalities in the digestive, nervous system.
- Inflammatory bowel disease: A group of digestive disorders which causes certain changes in the bowel tissue is regarded as inflammatory bowel disease. It may also increase the risk of colorectal cancer and two of its main causes are ulcerative colitis and Crohn’s disease. Both lead to inflammation in the digestive tract which in turn causes pain in the abdomen.
Causes Specific to Women
There are a few reasons that are specific to women and cause pain on the right side of the abdomen. These factors are usually more serious and require medical attention. Even though the pain may be felt on the lower right side of the abdomen, the pain may be arising from the left side. Some of the common causes include:
- Menstrual cramps
- Endometriosis
- Ovarian cyst
- Ectopic pregnancy
- Pelvic inflammatory disease
- Ovarian torsion
Causes Specific to Men
Similar to women, few causes are specific to men only. These conditions require immediate medical attention and two major reasons include:
- Inguinal hernia
- Testicular torsion
When to visit the doctor?
The following symptoms are a cause for concern and require urgent medical attention:
- Chest pain or pressure in the chest
- Fever
- Blood in the stool
- Constant vomiting & nausea
- Jaundice
- Swelling in the abdomen
- Severe tenderness when you touch the abdomen
It is important to consult a doctor when the pain in the lower right abdomen lasts for more than a few days.
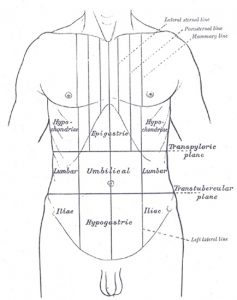
Abdominal Pain Illustration Image
The post Right Side Abdominal Pain | Causes, Symptoms, Diagnosis & Treatments appeared first on Prime Health Channel.
]]>The post Epigastric Pain | Causes, symptoms, diagnosis & Treatment appeared first on Prime Health Channel.
]]>Epigastrium lies in the upper abdomen precisely over the stomach. The epigastric region includes the stomach, a part of the liver, pancreas, and duodenum.
What is Epigastric Pain?
Epigastric pain occurs in the upper abdominal area just below the ribs. It occurs mainly when the gastric components tend to move upwards towards the back of the throat making a person feel a burning sensation and inflammation. The pain is usually felt while eating or right after eating or lying down immediately after eating. The nature of the pain might vary from mild to severe at times.
It is quite common in pregnant women as a result of increased pressure in the abdominal area and various hormonal changes that slow down the digestive process.
Causes of Epigastric Pain
Different disease can cause this pain, so it becomes quite difficult to find out the exact reason behind it. But the common Aetiologies are the following-
- Overeating
- Consumption of alcohol while eating
- Excessive spicy and rich foods
- Cancer in the gall bladders, pancreas or stomach
- Carcinoma of the stomach
- Cardiovascular issues such as heart attacks
- Gastroesophageal reflux disease (GERD) occurs due to the casting up of gastric acids into the esophagus leading to a burning pain
- Heartburn caused by large amounts of gastric acids secreted and refluxed back to the esophagus
- Peptic ulcers
- Gastritis (inflammation of the stomach lining)
- Duodenal ulcer
- Pancreatitis (acute or chronic)
- Hepatitis causing inflammation in the liver due to virus infection
- Stomach disorders may generate pain due to inflammation and infection
- Gastroenteritis
- Gallbladder stones or inflammation
- Abdominal aortic aneurysm
- Continuous coughing turns chronic and may lead to pain
- Abdominal muscle strain lead to epigastric pain
- A hiatal hernia also cause pain in the epigastrium
Symptoms of Epigastric Pain
The pain may come along with other symptoms of the underlying disorder or the original disease. But, it may involve other symptoms like:
- Heartburn
- Abdominal pain
- Indigestion
- Swelling in the abdomen
- Abnormal acidic taste in your mouth
- Frequent belching
- Throat soreness or hoarseness
- Constipation
- Feeling a lump in your throat
- Ongoing cough
- Burning sensation in the abdomen or chest area
- Diarrhea
- Nausea and vomiting
- Gas problems
A few cases of epigastric pain may be symptoms of an upcoming heart attack or other life-threatening hazards:
- Chest pain, tightness and pressure in the chest, even palpitations
- Pain moving down the shoulder and arm
- Difficulty in breathing may also lead to choking
- Presence of blood or black components in vomiting
Diagnosis for Epigastric Pain
The doctor initially examines the patient’s history and conducts a physical examination along with a few tests to diagnose the actual cause:
- Complete blood count test for determination of levels of hemoglobin & blood cells count
- Blood test for the evaluation of liver & pancreatic enzymes
- ESR (Erythrocyte Sedimentation Rate) to detect the rate of inflammation in the body
- Abdominal X-ray is a must to check if there is any obstruction or mass
- Endoscopy for assessment of problems in the esophagus such as inflammation or growth of mass
- Urinalysis to detect urinary tract infection
- Ultrasound test or CT scan
- Cardiac tests are also recommended to check if the heart is involved in the pain
Treatment for Epigastric Pain
A few cases of epigastric pain might not need any treatment if further complications do not occur. However, the treatment depends on the diagnosis and the underlying cause of the pain. The following might treat pains arising due to severe disorders:
- Antacids used to reduce excess of acids produced in the stomach
- Intake of H2 blockers for curing peptic ulcers and preventing the excess acid formation in the stomach
- Non-steroidal anti-inflammatory drugs (NSAIDs) might help in pain relieving and also to reduce inflammation and fever.
Home remedies
A doctor must be called in for Epigastric pain, but a few methods can be tried at home to redeem the pain. The following are-
- Aloe Vera juice diluted into other liquids treats various stomach problems
- Ginger tea may relieve stomach disorders by neutralizing the acid and reduce inflammation or irritation in the tissue of the digestive tract
- Baking soda with warm water helps to neutralize acidity
- Chamomile tea fights symptoms of epigastric pain, relieve heartburn and soothes the stomach
- Yoghurt for indigestion
- Eating burnt toast detoxifies the stomach
- Peppermint tea proves to be a proper remedy except for GERD
Complications associated with Epigastric Pain
Epigastric pain although harmless in most cases may cause serious complications if the symptoms deteriorate. It results in discomfort while eating and can affect eating habits causing a weight loss. Some of these hazards include-
- Cancer of esophagus, stomach, and other organs
- Scarring and narrowing of the Esophagus
- Heart attacks
- Poor nutrition due to less eating
- Weight loss
- Poor life quality
- Risk of cancer
- Infection
When to visit a doctor?
Epigastric pain does not usually cause such risks and might go away within an hour or two. But in serious cases, one must visit a doctor when the following symptoms are common:
- Continuation of pain more than one or two days
- Regular burning sensation and pain after eating
- Pain in the chest and stomach
- Regurgitation of acid in frequent interval
The post Epigastric Pain | Causes, symptoms, diagnosis & Treatment appeared first on Prime Health Channel.
]]>The post Appendix Pain appeared first on Prime Health Channel.
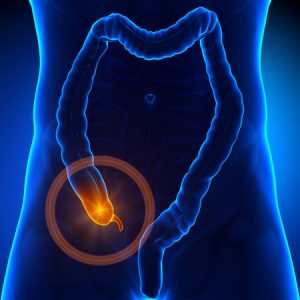
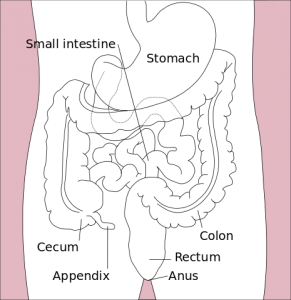
]]>The appendix is a small, thin pouch and worm-like structure that is present in the colon and connected to the large intestine. It is anatomically termed as the vermiform appendix which means worm-like. The appendix is located in the lower part on the right-hand side of the abdomen and is usually a closed-ended, narrow tubular tissue, i.e., about 5-10 cm (approximately 4 inches long).
What is appendix pain?
Appendix pain medically termed as appendicitis is a painful swelling of the appendix present in the cecum of the colon. If not appropriately treated on time, it might burst and be life-threatening. Pressing on that area, coughing or a walk may increase the pain making the situation worse. It can happen to any person at any point of time but is common more in men than women. Appendicitis occurs mostly between the ages of 10 to 30 years.
An appendix pain develops mainly in the middle of the abdomen which may appear and go but gradually moves to the lower part of the right-hand side of the abdomen. The pain becomes constant, and with time it becomes severe.
Causes of Appendix Pain
Appendicitis occurs due to blockage or any obstruction in the appendix due to a congregation of mucus or other parasites. It produces bacteria and rapidly multiplies as well as infects the intestinal wall. The growth of bacteria leads to inflammation and irritation causing pain that mostly begins in the middle of the abdomen that may appear or disappear at times. Other likely causes include:
- Cancer: Mostly rare, the presence of cancerous tumor might cause a blockage in appendix causing pain in that area.
- Infection: Any obstruction might eventually lead to an infection that makes the appendix inflamed as a natural reaction.
Signs & Symptoms of Appendix pain
- Mild pain at first near the navel or upper part of the abdomen
- Vomiting after the pain
- Nausea
- Swelling in the abdomen
- Loss of appetite
- Diarrhea
- High fever up to 102 degrees
- Constipation
- A feeling of tenderness in the abdomen.
- Difficulty to pass gas.
- Pain while urinating
- Severe cramps
Differentiating Appendicitis from Other Health Conditions
Sometimes it becomes difficult to diagnose appendix pain as the symptoms are quite similar to many other abdominal diseases which include:
- Problems in the gallbladder
- Infection in the bladders
- Urinary tract infections
- Crohn’s disease
- Gastritis, several intestinal infections
- Ovary ailments
- Onset of labor pain during pregnancy
Also, due to its variation in size, location and being nearly located to other organs in the abdomen, it is tricky to differentiate appendicitis from other pelvic and abdominal issues. Some other conditions that may be confused with appendicitis are:
- Pelvic inflammatory disease (PID)
- Diverticulitis mainly caused on the right side abdomen
- Meckel’s diverticulitis
- Liver diseases
- Duodenal ulcer
Diagnosis of Appendicitis
Some tests that are highly recommended for diagnosing appendix pain are:
- CT scan and ultrasonography
- White blood count test
- Examination to check if there is inflammation in the abdomen
- Abdominal X-ray
- Blood test to detect any infectious elements present
- Urine tests to recognize infections in the urinary tract
- Rectal examination
- Barium Enema
- Laparoscopy
Risks & complications due to appendix pain
- Inflammation tends to develop a lump or a structure in the right lower abdomen. This mass grows due to the scarring caused by the medicines used for healing and might increase the risk of cancer in the abdomen.
- Perforation is the most critical issue that may lead to a peri-appendiceal abscess (segregation of infectious pus). It may also lead to infections in the entire lining of the abdomen wall and the pelvis. The complication occurs mainly due to delay in diagnosis and proper treatment.
- Another severe complication occurs when the infectious bacteria enters the blood and affects other parts of the body too. This condition called sepsis is a rare yet very serious condition that can even be life-threatening.
- Blockage in the intestinal wall due to the inflammation around the appendix leads to compression of the intestine. Due to blockage, the intestine fills with gas and liquids with symptoms like nausea and vomiting.
Treatment
Surgery
At times, the appendix gets healed without surgery if the rupture happens with infection and inflammation. However, the symptoms may also go away with the use of antibiotics, especially in case of older people. As soon as the appendix gets diagnosed, it should be immediately removed by appendectomy to avoid the risk of an appendix burst. It is done under anesthesia either by a keyhole (laparoscopy) or open surgery. However, keyhole surgery is preferable as the patient recovers sooner than the open technique.
Alternatives to cure appendix pain
In case the lump or mass comprises of fatty tissue, it recovers and heals the issue on its own. However, if it is located during diagnosis, doctors might advise surgery wherein the patient is treated first with antibiotics and then operated a few weeks later. In some instances, the operation is not at all necessary, and the lump may disappear with medicines only.
Factors during Recovery after Surgery
After the surgery, you must keep an eye on the patient for various symptoms which are prone to cause further infection. They are as follows:
- Increased pain & swelling
- Repeated vomiting
- High fever
- Discharge from the area operated
- Wound is very sensitive to touch
How to prevent Appendix pain?
It is difficult to prevent appendix pain, but some foods may lower the risk. Intake of foods rich in fiber might lessen it. Fresh fruits and vegetables containing high fiber can help in preventing constipation and build up of stool which is the primary cause for appendicitis. Some high fiber items that may be helpful to avert it include:
- Apples
- Artichokes
- Pears
- Raspberries
- Green peas
- Lentils
- Broccoli
- Whole wheat spaghetti
- Oatmeal
- Bran flakes
- Black beans
- Barley
The post Appendix Pain appeared first on Prime Health Channel.
]]>The post Inflamed Colon appeared first on Prime Health Channel.
]]>Inflamed colon known as Colitis in medical terms is a disorder caused in the intestines (both large & small intestines) that cause abnormalities and bowel diseases.
Types of Inflamed Colon
Crohn’s disease
A part of the gastrointestinal tract gets inflamed by this type of colitis. The tail end of the small intestine is mostly affected, but it can affect all the layers of the bowel. It causes inflammation and creates patches across different parts of the digestive tract.
Ulcerative colitis
It acutely affects the large intestine causing the lining of the colon to develop ulcers and sores that excrete pus and mucus at times. It causes inflammation in the intestine and abdominal discomfort. It also causes a continuous inflammation in one particular area and results to affect deeper into the intestine.
Diverticulitis
It occurs when the outer lining of the bowel pouches out through the layers of the spots present in the muscles of the intestinal wall. As a result of this, inflammation or infection is caused in the digestive tract. The small pores face obstruction from parts of stool and other infectious materials. The nearest tissue of the colon present on the left-hand side is inflamed and thereby causes pain and even fever. However, this can be treated by antibiotics. If not treated through medication, the condition worsens further leading to leakage of the colon and moreover blockage of the bowel. In that case, surgery is a must to remove the affected area of the intestine.
Antibiotic-Associated Colitis
The colon usually consists of natural and healthy bacteria. Intake of antibiotics for treatment of any disease might kill these useful bacteria thereby allowing the other harmful bacteria to affect the colon causing inflammation. The most common type is named Clostridium difficile and it generates the disease called antibiotic-associated colitis. In case it is mild, it may be healed by taking metronidazole orally. In moderate cases, it can be treated by vancomycin which is also taken orally. But in acute conditions, the patient should be medicated with a mixture of oral vancomycin and metronidazole generated through a vein and vancomycin enemas. But when it comes to more severe issues such as bowel rupture, surgery is advised. Again, some complicated cases of this disease can be overcome by fecal pellets donated to the patient.
Chemical Colitis
When chemicals get inserted into the colon, the colon gets inflamed, and major damages can occur. The mucosal lining of the colon might also get inflamed when reacted to strong chemicals.
Medication-associated colitis
Inflamed colon can also be the effect of intake of several medicines such as NSAIDs (nonsteroidal anti-inflammatory drugs), mycophenolate, ipilimumab and retinoic acid.
Causes of Inflamed Colon
Collagenous colitis intermed mag (Inflamed colon)
Colitis tends to occur more in younger people than the aged ones. The major causes are as follows:
- Bacteria: One of the vital causes, most of these enter the human body through food and causes disorders, food poisoning or other stomach infections.
- Parasite infections: A significant cause of infectious colitis, it mainly occurs due to contamination of water. Infected water causes serious issues.
- Pseudomembranous colitis: Mainly caused by a specific bacterial infection known as Clostridium. People taking antibiotics or admitted at the hospitals tend to suffer from this kind of colitis. Most antibiotics kill the good bacteria and replace them with the Clostridium bacteria causing diarrhea along with fever.
- Lack of Supply of Blood: Arteries which supply blood to the colon sometimes tend to narrow themselves. As a result, the required amount of blood fails to enter the colon causing inflammation. Lack of blood supply in the human body can cause abnormal bowel movements containing blood, abdominal pain and also fever.
Symptoms of Inflamed Colon
- Fever sometimes accompanied with chills
- Frequent bowel movements
- Loss of appetite
- Considerable weight loss
- Diarrhea (sometimes with the presence of blood)
- Abdominal pain or cramps
- Feeling tired and restless
- Constipation
- Muscular spasms
- Deficiency of iron
Diagnosis of Colitis
Some tests and diagnostic methods are to be carried out, they include:
- Blood test
- Stool test
- Colonoscopy (endoscopy using camera to provide the entire view of the colon and the surrounding part)
- Biopsy should be undergone to collect a small sample of the tissue for diagnosis
- Video capsule endoscopy
- CT scan
- Special X-ray named small bowel fellow
- Enterography is done to find out if there is inflammation
Treatments for colitis
There is no immediate treatment for this, and the general procedure is to lessen the signs and symptoms. Doctors may suggest a drug therapy, and if not cured, the ultimate step is to undergo surgery. A few mild medicines may be prescribed.
Some common drugs that are used to reduce the symptoms are as follows:
- Antibiotics (prescribed to control the disease and prevent it from spreading)
- Anti-inflammatory drugs (usually used to prevent the inflammation)
- Immunosuppressant (Helps to prevent further irritation in the colon)
Natural home remedies
- Have smaller meals at intervals throughout the day at least five to six times
- Taking multivitamins and minerals can help as inflamed colon causes a lack of nutrients
- Smoking should be avoided to minimize the risk of inflammation
- Limit stressful situation and reduce mental stress by simple exercising to reduce depression
- Yoga and meditation might also help
Recommended foods to reduce Colitis
- Drink enough amounts of fluids as the body gets dehydrated during diarrhea
- Include probiotics like cheese and yogurt in your diet
- Soluble fiber foods, barley, grains and peeled fruits are equally helpful
Foods to Avoid
- Prefer steamed or boiled vegetables instead of eating them raw
- Fruits like berries and pineapples
- Avoid having whole grains such as oatmeal, nuts or seeds
- Avoid eating cooked greens like cabbages or corn
- While having meats try to stew them and make it softer
- Avoid alcoholic drinks too, instead drink lots of water and sports’ drinks
- Stay away from spicy foods which can irritate the bowel movement
- Tea, coffee, dairy products and even chocolate is a strictly a no-no
Prevention of Inflamed Colon
- Primary reasons are the inadequate supply of proper and clean drinking water, unhygienic sanitation leading to affect thousands of people even causing death. Also in the developed nations, poor conditions of hand washing and kitchen hygiene bring in infectious colitis. So the primary way to prevent it is to maintain cleanliness everywhere.
- On the other hand, inflammatory bowel disorders might be problematic to deal with as they are hereditary. It also generates an abnormal auto-immune response to an unidentified stimulus in the body.
- Ischemic colitis occurs when the blood vessels connecting to the bowel begin to narrow. This condition lowers the risk for other types of circulatory disorders like peripheral vascular disease, heart attack and even resulting in a stroke. The primary reasons are smoking habits, high blood pressure, high levels of cholesterol and diabetic tendency too.
When to visit a doctor?
If any of the following symptoms arise, a doctor must immediately be informed:
- Temperature above 101°F or fever along with chills
- Stools containing blood most of the times
- Lightheadedness, rapid heart rate or frequent passing out
- Frequent vomiting
- Severe abdominal pain at times with bloating.
- Acute dehydration causing minimum or no urine for almost 12 hours or more
- Secretion of pus from around the anus
- Pain and swelling in the anal area
- No excretion of stools
The post Inflamed Colon appeared first on Prime Health Channel.
]]>The post Collagenous colitis appeared first on Prime Health Channel.
]]>Collagenous colitis is an inflammatory disease of the colon, which is related with watery and chronic diarrhea, but without blood [1]. It is one form of microscopic colitis, the other being lymphocytic colitis.
Collagenous colitis Incidence
The incidence is high in industrialized countries like United States, Canada, Europe, New Zealand and Australia. Estimates indicate that the incidence has increased from one to approximately 19 in every 100,000 individuals. The prevalence increases with age and peaks in people in their 70s [2].
Collagenous colitis Symptoms
These involve:
- Intermittent bouts of diarrhea
- Painful abdominal cramps
- Multiple episodes of loose, watery bowel movements every day
- Dehydration and fatigue (acute cases)
Such episodes may arise abruptly, without any apparent reason [3].
Collagenous colitis Etiology
The exact causes are unclear [4]. As per some unproven theories, the underlying factors might be:
- Some auto immune disorder
- Damage from food poisoning
- Association with NSAIDs or non-steroidal anti-inflammatory medications (Ibuprofen etc.)
Around half of all sufferers can identify the particular time of occurrence of the first bout.
Associated disorders
These involve:
- Coeliac disease
- Lymphoma
- Autoimmune disorders like thyroid disease and rheumatoid arthritis (as seen in 20-60% sufferers)
Collagenous colitis Risk Factors
Adults over 40 years of age are usually the most risk-prone. People suffering from an autoimmune disorder are also regarded as susceptible by doctors [5].
Collagenous colitis Diagnosis
Diagnosis involves:
- Physical examination
- Analysis of medical history
- Laboratory analysis of stool and blood samples (often yielding normal findings)
A series of diagnostic tests are often ordered to ascertain the exact cause/causes. These involve:
- Scope test (sigmoidoscopy, colonoscopy etc.)
- Microscopic examination of colonic biopsies [6]
Collagenous colitis Differential Diagnosis
Biopsies of the colon should be examined under microscope to avoid misdiagnosis as irritable bowel syndrome (IBS) or lymphocytic colitis.
Collagenous colitis Treatment
Despite multiple management and curative options being present, no single treatment option is regarded as effective for Collagenous colitis. Treatment only aims at reducing inflammation and diarrhea symptoms. Treatment options include:
Medications
These include:
- Anti-inflammatory agents like Azulfidine (sulfasalizine) or Asacol (mesalamine) [7]
- Steroid drugs like Prednisone or Entocort
- High dose Pepto-bismol
- Drugs like Imodium (loperamide) and Lomotil (diphenoxylate), to treat diarrhea
- Cholestryramine, to limit diarrhea
- Antibiotic therapy (Flagyl, penicillin and erythromycin)
Probiotics (Healthy bacteria)
Acidophyllus (found in yogurt), Florastor and Culturelle help restore the balance of beneficial bacteria inside the colon.
Diet
Although no specific diet is recommended, patients should avoid lactose or caffeine to avoid fluid secretion in the colon. Low-fat diets should be followed in the event of inability to digest fats.
Surgery
Radical surgery (for colon removal and creating a diverting ileostomy) is a possible cure, but is mainly reserved for acute cases and is seldom recommended.
Home Remedies
These include:
- Drinking lots of fluids (rich in sodium and potassium), watered-down fruit juice or broth
- Consuming soft foods (like rice, bananas or applesauce)
- Eating multiple small meals than a single large meal
Collagenous colitis Complications
The possible complications include:
- Weight loss
- Severe dehydration
- Vitamin deficiency
- Loss of bone density and hypertension (due to long-term steroidal treatment) [8]
Can Collagenous colitis kill you?
It is not life-threatening. However, there are cases that need intensive resuscitation – particularly those associated with vitamin deficiency, weight loss and acute dehydration.
Collagenous colitis Prognosis
Symptoms usually recur when treatment is slowed down. Most patients require continual therapy for management of the symptoms. The long term outcome varies, with some sufferers showing quick response and others taking time. There is also a waxing and waning period of symptoms. Continued treatment usually reduces problems.
Collagenous colitis Prevention
Worsening of the symptoms can be prevented by measures like:
- Non-intake of irritating foods (fried, or rich in fat or spicy foods are to be avoided)
- Avoiding beverages like alcohol, caffeine or tea (high in sugar) [9]
As the exact cause is unknown, the condition itself cannot be prevented.
Although often difficult to cure completely, Collagenous colitis can be managed with proper medical assistance as much as to make a better quality of life possible for sufferers.
The post Collagenous colitis appeared first on Prime Health Channel.
]]>The post Cyclic Vomiting Syndrome appeared first on Prime Health Channel.
]]>Cyclic Vomiting Syndrome (CVS) is a functional vomiting disorder characterized by cycles or episodes of acute nausea and vomiting that persists for several days or hours and alternate with asymptomatic episodes [1].
It is also called:
- Abdominal Migraine [2]
- Periodic Syndrome
- Childhood Cyclic Vomiting
- Cyclical Vomiting Syndrome
- Chronic Vomiting in Childhood
Cyclic Vomiting Syndrome Epidemiology
The exact prevalence and incidence of CVS is unknown. In a region in central Ohio with mainly white population, the prevalence of CVS in kids was found to be 0.04% [4].
Cyclic Vomiting Syndrome Symptoms
The signs and symptoms include:
Cyclic vomiting
It may be characterized by either severe vomiting occurring several times every hour and lasting for less than a week, or 3 or more distinct episodes of vomiting without any apparent cause in the last 1 year.
Vomiting episode
It is typically characterized by fever, diarrhea, abdominal pain, dizziness and sensitivity to light.
The intervals between vomiting episodes are usually asymptomatic. However, some patients may suffer from the following problems between episodes:
- Abdominal pain
- Limb pain
- Anxiety
- Depression
- Mild to moderate nausea
Dehydration
Constant vomiting can result in severe dehydration which can be fatal for sufferers. The symptoms include:
- Paleness
- Thirst
- Less urination
- Listlessness
- Exhaustion
Cyclic Vomiting Syndrome Risk Factors
The risk factors include:
Having migraines
Children with a family history of migraines are found to suffer from CVS when they get older. The relationship between CVS and migraines is not clear.
Long-term marijuana use
Chronic usage of marijuana (cannabis sativa) has also been linked with the development of CVS.
Cyclic Vomiting Syndrome Etiology
The exact causes of CVS are not known. The trigger factors for vomiting episodes are:
- Hot weather
- Menstruation
- Motion sickness
- Physical exhaustion
- Foods, such as cheese or chocolate
- Colds, allergies or sinus problems
- Overeating or eating just before going to bed
- Panic attacks or anxiety, particularly in adults
- Excitement or emotional stress, especially in children
Identifying the trigger factors for CVS may help manage its symptoms.
Cyclic Vomiting Syndrome and Genetics
Heredity (mitochondrial inheritance) is supposed to play a role in CVS development, as the disease is found to have a possible relationship with migraine. Single-base pair and rearrangements in mitochondrial DNA have been linked with these attributes.
Cyclic Vomiting Syndrome Diagnosis
Diagnosis can be difficult for CVS. Diagnostic procedure usually involves:
- Asking about the symptoms
- Consideration of medical history
- Physical examination
Diagnostic tests may involve:
- MRI scans, to detect brain tumor and other central nervous system disorders
- Imaging studies (like CT scan, endoscopy, magnetic resonance imaging), to detect digestive system obstructions and other disorders
- Lab tests, to detect metabolic disorders and thyroid conditions
- Motility tests, to detect digestive disorders and monitor food movement through the digestive system
However, there are no specific tests for CVS.
Cyclic Vomiting Syndrome Diagnostic Criteria
The essential diagnostic criteria for CVS include:
- A history of 3 or more periods of unremitting vomiting and severe nausea, and pain (in some cases), that lasts for a few hours, days or even weeks or months
- Intervening asymptomatic intervals, which persist for weeks to months
- Exclusion of gastrointestinal, metabolic, or biochemical or structural disease of CNS (central nervous system)
Cyclic Vomiting Syndrome Differential Diagnosis
In order to avoid misdiagnosis, the differential diagnosis should include isolating the signs of CVS from those of:
- Gastrointestinal (GI) disorders (Gastroesophageal reflux disease, Inflammatory bowel disease etc.)
- Neurologic disorders (Abdominal migraine, Migraine headaches etc.)
- Renal disorders (such as Nephrolithiasis)
- Metabolic disorders (Mitochondriopathy, Urea cycle defects etc.)
- Endocrine disorders (Addison disease, Pheochromocytoma etc.)
Cyclic Vomiting Syndrome Treatment
There is no cure for CVS. Treatment aims at controlling the symptoms. Medications prescribed include:
- Anti-nausea drugs
- Antidepressants
- Sedatives
- Drugs that suppress stomach acid
Drugs used to manage migraine problems can sometimes prevent or stop cyclic vomiting episodes. The medicines may be recommended for frequent and chronic episodes.
Acute cases of dehydration may need treatment in hospital.
Cyclic Vomiting Syndrome and Behavioral Therapy
As per research, around half of all CVS sufferers have anxiety or depression. It is unclear to what extent anxiety and depression can result from, or cause, cyclic vomiting. Behavioral therapy (involving techniques and exercises) may be recommended for children suffering from anxiety or depression.
Cyclic Vomiting Syndrome Home Remedies
Home remedies for CVs include measures like:
- Getting enough sleep
- Resting in a quiet place in between vomiting bouts
- Drinking enough water to restore electrolyte balance
- Eating solid foods only after feeling better
- Reducing stress
- Eating small meals
Cyclic Vomiting Syndrome – Alternative Medicines and Cure
These involve:
- L-carnitine (natural substance that assists in fat-to-energy conversion)
- Coenzyme Q10 (ubiquinone), which helps in basic cellular functions
Stress, which can trigger vomiting bouts, can be managed by Biofeedback training.
However, none of these have been studied well.
Cyclic Vomiting Syndrome Complications
The complications for CVS include:
- Tooth enamel decay, caused by acid in vomit
- Dehydration, caused by loss of water due to excessive vomiting
- Injury to the esophagus, caused by stomach acid
Cyclic Vomiting Syndrome Prevention
Avoiding trigger factors can reduce the frequency of vomiting bouts. Prevention can also include lifestyle modification measures like:
- Getting proper sleep
- Avoiding trigger foods (chocolate, cheese etc)
- Eating small meals and snacks daily at regular intervals
Cyclic Vomiting Syndrome Prognosis
CVS persists for an average span of 2- 2.5 years. It resolves in late childhood or during early teen years. A few patients continue to exhibit symptoms even when they turn into adults.
Can Cyclic Vomiting Syndrome Kill You?
There is little evidence of mortality associated with CVS. However, acute cases of fluid loss can cause potentially fatal salt imbalances. During a CVS episode, blood pressure increases dangerously (hypertension). Severe dehydration due to CVS, that goes untreated, can also cause death.
Cyclic Vomiting Syndrome Support Groups
Patients can get information and assistance from various support groups and online forums. These include (5):
National Organization for Rare Disorders
55 Kenosia Avenue
P.O. Box 1968
Danbury, CT 06813–1968
Phone: 1–800–999–6673 or 203–744–0100
Fax: 203–798–2291
Email: [email protected]
Internet: www.rarediseases.org
Cyclic Vomiting Syndrome Association
2819 West Highland Boulevard
Milwaukee, WI 53208
Phone: 414–342–7880
Fax: 414–342–8980
Email: [email protected]
Internet: www.cvsaonline.org
Cyclic Vomiting Syndrome ICD9 Code
The ICD9 Code for CVS is 536.2 [3].
The post Cyclic Vomiting Syndrome appeared first on Prime Health Channel.
]]>The post Short Bowel Syndrome appeared first on Prime Health Channel.
]]>Short Bowel Syndrome (SBS) is a condition characterized by malabsorption of nutrients which occurs as a result of surgical removal of the small intestine, or in some rare cases – due to complete dysfunction of major portions of the bowel. It is a rare condition caused by either acquired or congenital factors. It may affect both children and adults.
The condition is also referred to by other names, such as Short Gut Syndrome or simply Short Gut.
Short Bowel Syndrome Epidemiology
Studies on the incidence and/or prevalence of this condition are not easy to make due to its rarity. In the UK, the average number of patients was 2 in per million, based on the number of individuals requiring long term home parenteral nutrition. In Spain, the affected population was nearly 1.8 in per million (as recorded in 2002).
Short Bowel Syndrome Causes
SBS can be caused by various acquired or congenital factors, which include:
- Gastroschisis
- Tumors of small intestine
- Trauma or injury to small intestine
- Bypass surgery for treating obesity
- Necrotizing enterocolitis in premature newborns
- Crohn’s disease, which is an inflammatory disease of digestive tract
- Surgery to get rid of diseases or damaged portions of the small intestine
- Volvulus, a condition which involves spontaneous twisting of small intestine that shuts off blood supply, leading to death of tissue
Short Bowel Syndrome Symptoms
The symptoms of SBS include:
- Fatigue
- Diarrhea
- Weight loss
- Malnutrition
- Fluid depletion
- Abdominal pain
- Abdominal bloating
- Swelling or edema, primarily of the legs
- Steatorrhoea, accompanied by malodorous stools
SBS patients may also exhibit complications that are caused by insufficient absorption of minerals and vitamins, such as vitamins A, E, D, K and B12 as well as calcium, iron, magnesium, zinc and folic acid. These may give rise to symptoms of:
- Anemia
- Hyperkeratosis or scaling of skin
- Muscle spasms
- Easy bruising
- Bone pain
- Poor blood clotting
Short Bowel Syndrome Diagnosis
The following tests are normally conducted to detect whether or not a child or an adult is having this syndrome:
- CT scans
- Endoscopy
- Liver biopsy
- Electrolytes
- Fecal fat test
- Colonoscopy
- Creatinine tests
- CT enterography
- Abdominal x-rays
- Stool sample tests
- Coagulation profile
- Bone densitometry
- Indirect calorimetry
- Blood chemistry tests
- Vitamin levels in blood
- Abdominal ultrasounds
- Breath hydrogen analysis
- X-rays of the small intestine
- Complete blood count or CBC
- Serum levels of magnesium, calcium and phosphorus
Short Bowel Syndrome Differential Diagnosis
A number of conditions show signs and symptoms similar to that of SBS. Hence, while determining the presence of SBS, a doctor needs to differentiate it from these similar disorders. The differential diagnosis of SBS includes distinguishing its signs from those of other conditions such as:
- Coeliac disease
- Anorexia nervosa
- Bacterial overgrowth
- Active Crohn’s disease
- Small bowel malignancy
- Other factors leading to chronic diarrhea, malabsorption and growth failure
Short Bowel Syndrome Associated Conditions
A number of diseases are closely associated with SBS. These include the following:
- Trauma
- Gastroschisis
- Crohn’s disease
- Intestinal atresias
- Radiation enteritis
- Intestinal volvulus
- Meconium peritonitis
- Necrotising enterocolitis
- Ischaemic bowel infarction
- Congenital short small bowel
- Mesenteric vascular accidents
- Recurrent intestinal obstruction
Short Bowel Syndrome Treatment
At present, there are no definite curative options for SBS. Treatment for SBS is primarily aimed at relieving the symptoms. Prescription medications may be administered to manage the condition which includes:
- Anti-diarrheal medicines like Loperamide and Codeine
- Mineral supplements, vitamins and L-Glutamine powder intermixed with water
- Proton pump inhibitors and H2 blockers to reduce the amounts of stomach acids
- Lactase supplements, which can improve symptoms of bloating and diarrhea that are connected with lactose intolerance
- Folic acids, vitamin B12 and dietary irons to treat anemia
- Intravenous supplements of minerals and vitamins
- Imodium, to control the symptoms of diarrhea by giving the small intestines adequate time to absorb nutrients and water
- Ursodeoxycholic acid, that can prevent and/or dissolve cholesterol gallstones
- Oral antibiotics, that can prevent or cure overgrowth of small bowel bacteria
- Medications that can slow down normal movement of intestines
- The agent teduglutide, which is a glucagon-like peptide-2 analog that is developed by the NPS Pharmaceuticals
The medications should also be accompanied by a high-calorie diet that supplies all the necessary minerals and vitamins as well as various types of fats, proteins and carbohydrates.
Nutritional Management
As the intestines of SBS patients are not able to absorb adequate amounts of nutrients, doctors may recommend administering intravenous or tube feeding. These procedures are:
Parenteral Nutrition (PN)
Parenteral Nutrition involves administration of a specially-made nutritional formula directly into the patient’s bloodstream with the help of intravenous channels (IV). The formula is carefully prepared by the dietician to meet the specific energy needs of the patient. Delivering the nutrients straight to the bloodstream also allows to bypass the involvement of the digestive system altogether.
The special formula is generally administered daily over a course of 12-24 hours. If the patient requires a long-term PN support, the length of such a session will be reduced gradually.
Enteral Nutrition (EN)
In this procedure, the nutritional formula is administered through a tube. It is also referred to as tube feeding. This can be accomplished in two ways:
- Using a Gastrostomy tube or G-tube that is passed through the opening into the stomach of patients
- Using a Jejunostomy tube or J-tube that is passed through the opening into a small portion of the small intestine
Surgery
The decision to settle for surgical operation on a SBS patient requires fine judgment. A surgery is undertaken only after careful consideration and after all the other therapeutic options has been exhausted. Some patients may require operation due to the complications presented by stasis of the enteric contents, bacterial overgrowth and prolonged parenteral nutrition.
It is sometimes possible to use surgery to reshape the small intestine of patients to increase surface area of intestines and prolong the duration of time required for the food to pass through, thereby giving intestines more opportunity to extract nutrients.
Common surgical procedures to manage SBS include:
STEP procedure
The STEP procedure was developed in early 2000s by MDs Tom Jaksic and Heung Bae Kim of the Children’s Hospital Boston. It involves lengthening of the bowel of patients which allows avoiding the necessity for intestinal transplantation. The process also creates a narrow space that allows the food to move through the digestive tract at an appropriate pace and carries bacteria and/or waste products out of the body.
Bianchi procedure
The Bianchi procedure also lengthens the dilated bowel by cutting one half of the bowel and sewing it to the other half.
Patients who do not respond well to the above-mentioned treatment procedures might be required to undergo an intestinal transplant. A number of transplant types exist, which include:
- Intestinal transplant
- Intestinal/liver transplant
- Multivisceral transplant; which involves removal of the intestines along with liver, spleen and the stomach on certain occasions
Short Bowel Syndrome Diet
SBS patients should avoid sodas, sugary desserts and fruit juices as these may increase the risk of diarrhea. Intake of salt may be increased depending on the status of the bowel. Diet for these patients depends on their condition. A diet with higher fat content is recommended for patients having 100 centimeters of jejunum intact, closing to nearly 50% or 60%. Carbohydrates should make up 20% to 30% of total daily calorie intake. Daily consumption of fibers should be limited to 15 grams or less. Lactose should be minimized or removed from diet if the patient is having lactose intolerance. The calcium levels should be kept at appropriate levels to lower the chances of Osteoporosis. An oral rehydration solution might be required due to difficulties in sodium absorption. The patient should also avoid bowel stimulants like alcohol and caffeine. The diet should also be supplemented by vitamin supplies. Chewing the food properly and adequately is necessary to facilitate nutrient absorption.
Short Bowel Syndrome Complications
A number of complications might emerge from SBS. These include:
- Gallstones
- Weight loss
- Malnutrition
- Renal failure
- Hemorrhage
- Wound sepsis
- Kidney stones
- Bowel necrosis
- Bowel obstruction
- Pulmonary embolism
- Anastomotic disruption
- Acute rejection of the transplant
- Osteomalacia or weakened bones
- Chronic rejection of the transplant
- Bowel dysfunctions and dysmotility
- Postoperative pulmonary dysfunction
- Metabolic acidosis caused by diarrhea
- Bacterial overgrowth in small intestine
- Hepatic, mesenteric or portal vein thrombosis
- Lymphoproliferative malignancies or disorders
- Thrombosis precluding sufficient access for feeding
- Infections associated with the venous feeding catheter
- Systemic sepsis with opportunistic organisms or ordinary pathogens
- Stasis of the intestinal contents without or with bacterial overgrowth
- Nervous system problems that are caused by low levels of vitamin B12
- Complications related to any of the underlying conditions, such as liver disease
Short Bowel Syndrome Prognosis
As there are no cures for this condition, survival of the patient and overall outcome may depend on a number of factors. The most common reason for death is liver failure which occurs after chronic hepatic parenchymal damage. The 4-year survival rate of newborn infants on TPN is approximately 70%. The 5-year survival rate is close to 20% in the same population with lower than 10% expected intestinal length. Many individuals die due to reduced venous access or severe septic complications. Pharmacological bowel compensation can help patients to avoid long term parenteral nutrition. Studies suggest that non-transplant surgical procedures can lead to clinical improvement of the condition in about 80% of patients. Early postoperative complications might lead to a higher mortality rate. However, 80% to 90% of patients who survive this critical stage are alive even after one year and almost 60% is alive after 4 years.
References:
http://www.patient.co.uk/doctor/Short-Bowel-Syndrome-%28SBS%29.htm
http://www.childrenshospital.org/az/Site1581/mainpageS1581P0.html
http://en.wikipedia.org/wiki/Short_bowel_syndrome
http://www.nlm.nih.gov/medlineplus/ency/article/000237.htm
The post Short Bowel Syndrome appeared first on Prime Health Channel.
]]>The post Alcoholic Hepatitis appeared first on Prime Health Channel.
]]>It is an inflammatory condition or hepatitis of the liver that is caused by an excessive consumption of alcohol. The condition is frequently found in close association with hepatosteatosis, which is an early phase of alcoholic liver disorder. It may significantly contribute to the progressive development of fibrosis, which can ultimately lead to cirrhosis. Common symptoms of this condition include jaundice, fatigue, ascites and hepatic encephalopathy. The mild cases of this liver hepatitis are usually self-limiting. However, the severe cases carry a high mortality risk.
Alcoholic Hepatitis ICD-9 Code
The ICD-9 Code for this disease is 571.1.
Alcoholic Hepatitis Causes
This form of hepatitis occurs when the liver is damaged due to excessive drinking of alcohol. The exact mechanism in which alcohol damages the liver and the reason why it affects only a small minority of regular heavy drinkers is not known. It is, however, clear that the process responsible for breaking down ethanol (the alcoholic compound present in wine, beer and liquor) produces highly toxic chemical substances like acetaldehyde. Chemicals like these trigger inflammations that destroy the liver cells. Web-like scars or small tissue knots develop over time that replaces the healthy liver tissue, thereby interfering with the natural functioning of the liver. This irreversible scarring, known as Cirrhosis, is the last stage of this alcoholic liver hepatitis.
Heavy consumption of alcohol can give rise to liver disorders, and the dangers increase with the total duration of time as well as the amount of alcohol consumed. However, as many heavy drinkers do not develop the symptoms of cirrhosis or alcoholic hepatitis in their entire lives, it is believed that certain other factors may play an important part as well. These include:
Obesity
Individuals with increased body weight are found to be more prone to this condition.
Malnutrition
Many heavy drinkers are actually malnourished people. This is either because they eat food poorly or that the alcohol and its harmful byproducts made it difficult for the body to absorb the food properly and break down its nutrients. This is especially so in case of certain vitamins, proteins and fats. Lack of nutrients caused by both these instances contributes to the cellular damage of the liver.
Genetic factors
Mutations of certain genes can affect alcohol metabolism. This may increase the risk of developing an alcoholic liver disorder, along with other complications such as alcohol-related cancerous conditions. The exact genetic propensities have not been identified yet.
Other forms of hepatitis
Presence of other forms of hepatitis can increase the risk of developing cirrhosis and liver hepatitis in a person if he or she is also found to be a heavy drinker. Hepatitis C greatly increases the risk of development of serious liver conditions.
Alcoholic hepatitis is not a viral condition and hence it is not contagious.
Alcoholic Hepatitis Risk Factors
There are certain risk factors that might increase the chances of an individual of developing this disorder:
- The quantity of alcohol consumed can be described as the most essential factor in determining the possibilities of an alcoholic liver disease.
- Women are slightly more prone to developing alcoholic hepatitis as compared to men. The difference might actually be related to the processing of alcohol by the two sexes.
- Certain genetic influences might predispose an individual to Alcoholic hepatitis.
- Hispanic and African-American individuals carry a higher risk of developing this condition.
- The type of alcoholic beverage one prefers more to drink might also influence the possibility of having this disease. For example, spirits and beers are riskier compared to wine.
- Binge drinkers make up a vulnerable population, so are obese people. The combined effect of alcohol and obesity is much more damaging than either of them operating alone.
Alcoholic Hepatitis Pathophysiology
Some of the signs and pathological alterations, observed in liver histology, consist of:
Ballooning degeneration
The hepatocytes, under the influence of alcoholic change, frequently swell up with excess amounts of fats, proteins and water. All these proteins are generally exported into the bloodstream of an individual. Necrotic damage is accompanied by ballooning. The swelling can block the nearby biliary ducts, which leads to Diffuse cholestasis.
Mallory’s hyaline
It is a condition that is characterized by accumulation of pre-keratin filaments in hepatocytes. Although this symptom is not exactly limited to the alcoholic liver disease, it is frequently a notable feature.
Inflammation
Necrotic changes trigger neutrophilic invasion as well as presence of the cellular debris within lobules. Generally, the Kupffer cells remove the quantity of debris. However they become overloaded in an inflammatory setting, thereby allowing the other white blood cells to get into the parenchyma.
The presence of chronic liver disease might indicate:
- Fibrosis
- Cirrhosis
Symptoms of Alcoholic Hepatitis
A number of different signs and symptoms are commonly associated with alcoholic hepatitis. This may include:
- Malaise
- Enlargement of liver
- A modest rise in the levels of liver enzymes
- Development of ascites or fluid in the abdomen of patient
The cases of Alcoholic hepatitis may vary from being mild showing only liver enzyme elevations to severe liver inflammations that accompany development of jaundice, a prolonged prothrombin duration as well as liver failure. The severe instances are marked by either obtundation or dulled consciousness or a combination of prolonged prothrombin time and elevated bilirubin levels. In both of the severe categories, the mortality rate is 50% within the first 30 days from onset.
Other symptoms of the condition include:
- Nausea
- Vomiting
- Weight loss
- Loss of appetite
- Encephalopathy
- Malnourishment
- Abdominal tenderness
Alcoholic hepatitis is different from cirrhosis that occurs as a result of long-term alcohol consumption. Patients having chronic alcoholic liver disorder and alcoholic cirrhosis might get affected by alcoholic hepatitis. The condition of Alcoholic hepatitis does not itself lead to cirrhosis. However, cirrhosis is more prevalent in patients who have been heavy drinkers of alcohol for a long time. Some alcoholic individuals develop the condition of acute alcoholic hepatitis as a sort of inflammatory reaction to cells that are affected by the fatty change. However, this is not something that is directly related to dosage of alcohol. Certain people seem to be more prone to have this reaction than the others. This is known as alcoholic steato necrosis.
Alcoholic Hepatitis Diagnosis
The diagnosis of this disorder is made in patients with a history of chronic alcoholism who develops worsening results of liver function tests. This includes elevated bilirubin levels and aminotransferases. Ratio between aspartate aminotransferase and alanine aminotransferase (AST/ALT ratio) is generally 2 or more. Under most circumstances, the liver enzymes do not exceed that of 500. The alterations on a liver biopsy are vital in confirming clinical diagnosis of alcoholic hepatitis.
The various tests conducted to diagnose this condition include:
- Electrolyte tests
- Complete blood cell count
- Blood tests for excluding other factors of liver disease
- Imaging tests, such as CT scan, MRI scan or ultrasound of the liver
- Liver function tests, such as total bilirubin, albumin and international normalized ratio
Alcoholic Hepatitis Differential Diagnosis
While diagnosing this disorder, physicians should rule out the presence of the following conditions that show symptoms similar to Alcoholic Hepatitis:
- Hepatitis C
- Hepatitis B
- Chronic Pancreatitis
Alcoholic Hepatitis Treatment
The treatment of this disease begins with the ceasing of alcohol consumption of the patient. Without it, other modes of curing the condition would not have any effect on the patient. According to the clinical practice guidelines recommended by American College of Gastroenterology, alcoholic hepatitis should be treated by administering corticosteroids. A Child-Pugh score or a MELD score should be used for risk stratification of the patients.
Patients with Hepatic encephalopathy or the ones showing a modified Maddrey’s discriminant function score greater than 32 should be treated with prednisolone 40mg tablets daily for 4 weeks which should be then followed by taper.
Randomized controlled trial indicated that patients showing at least 1 of the symptoms such as fever, palpable tender hepatomegaly, leukocytosis, hepatic systolic bruit or hepatic encephalopathy and having a discriminant function score greater than 32 should be treated with an oral dosage of pentoxifylline 400mg three times daily for four weeks in order to prevent death.
Liver transplant
In cases of severe alcoholic hepatitis, a liver transplant surgery might be the only remaining option to evade death. The survival rates for a transplant are similar to that of the other types of hepatitis which is greater than 70% for 5-year survival.
However, most medical centers are somewhat reluctant to perform this transplant surgery as they fear that patients would resume their drinking habits once surgery is complete. For most alcoholic hepatitis patients, the disease itself is considered to be a contraindication for the liver transplantation procedure in most of the transplant centers of US.
Treatment for malnutrition
Doctors might recommend certain dietary practices that patients might need to follow to reverse the nutritional deficiencies that accompany alcoholic hepatitis cases. A sufferer might also be directed to a dietician for assisting with his or her needs who may recommend an increased amount of vitamins or nutrients in the diet.
Alcoholic Hepatitis Complications
The following complications might result from Alcoholic hepatitis:
- Coma
- Jaundice
- Liver cancers
- Kidney failure
- An enlarged spleen
- Hepatic encephalopathy
- Varices or enlarged veins
- Scarring of liver or cirrhosis
- Ascites or accumulation of abdominal fluids
Alcoholic Hepatitis Prognosis
The long-term outcome for untreated cases of this condition is very severe. However, proper treatment and cessation of alcohol consumption can lead to a better recovery. If a patient of chronic alcoholic hepatitis continues to drink, he or she would inevitably develop symptoms of cirrhosis and liver failure. Death rate associated with alcoholic hepatitis is close to 50% within 7 years. Encephaylopathy, prolonged PT, PTT, kidney failure and ascites are promoting factors of liver failure. In some cases, death can also result from shock that is induced by the fat thrombosis within the lungs, very low levels of blood sugar or acute pancreatitis. Hence it is extremely important that a patient completely gets rid of his or her alcoholic tendencies if he or she has to have a positive outcome of treatment.
Alcoholic Hepatitis Prevention
The following guidelines can help an individual to protect himself or herself from getting infected by this condition.
- Alcohol should be consumed in moderate amounts, if at all.
- Certain medications come with a warning that they are not to be consumed with alcohol. Medications such as these like the pain killer acetaminophen should never be mixed with alcohol.
- Hepatitis C greatly increases the chances of developing alcoholic hepatitis for heavy drinkers. Hence exposure to the viral agent causing this disorder should be avoided. Care should be taken to avoid drug contamination or transmission of Hepatitis C through sexual contact.
Severe cases of Alcoholic hepatitis might lead to death. Patients need to cease drinking alcohol immediately after diagnosis as this can help in survival and recovery.
References:
http://www.mayoclinic.com/
http://edition.cnn.com/HEALTH/
http://emedicine.medscape.com/
http://nyp.org/health/liver-
http://medical-dictionary.
http://www.liverfoundation.
http://www.fpnotebook.com/gi/
http://en.wikipedia.org/wiki/
The post Alcoholic Hepatitis appeared first on Prime Health Channel.
]]>The post Lymphocytic colitis appeared first on Prime Health Channel.
]]>Lymphocytic colitis is a rare disorder that is characterized by chronic episodes of non-bloody watery diarrhea. It is a subtype of an inflammatory bowel disease known as microscopic colitis, the other being collagenous colitis. In this condition, colonoscopy reveals normal features. However, mucosal biopsy shows accumulation of lymphocytes within colonic epithelium and lamina propria connective tissue.
Lymphocytic Colitis Epidemiology
People who are diagnosed with lymphocytic colitis mostly fall within the age group of 60 to 80 years. Women are slightly more inclined to develop this disease than men.
Lymphocytic Colitis Causes
Medical experts are not sure as to what exactly causes this disease. However, some probable causes have been suggested which are discussed below:
Picture 1 – Lymphocytic colitis
- Long-term usage of drugs such as NSAIDs, antidepressants like Sertraline (Zoloft) as well as other medications.
- Viruses, which can trigger inflammations.
- Bacteria, that releases toxins which can irritate the colon lining
- Immune system problems in which the immune system destroys healthy tissues for no apparent reason; sometimes people having lymphocytic colitis also have another autoimmune condition, such as scleroderma, celiac disease or rheumatoid arthritis
Lymphocytic Colitis Symptoms
The main symptom of the condition is chronic, non-bloody diarrhea. Individuals having this form of colitis can have watery diarrhea for many months or even years before a conclusive diagnosis is made. The symptoms normally begin very slowly and steadily which are intermittent with periods of well being, followed again by spells of chronic diarrhea. Bloody stool is not usual. The overall signs and symptoms experienced by patients of the condition include other signs and symptoms such as:
- Fatigue
- Nausea
- Weight loss
- Bowel inconsistence
- Abdominal cramps or pain
- Abdominal bloating along with discomfort
Lymphocytic Colitis Diagnostic Criteria
The diagnostic criteria used to determine if a patient is suffering from lymphocytic colitis is presented below:
- Increased number of plasma cells, lymphocytes, mast cells and eosinophils are found in the colon’s lamina propria.
- Increased number of intraepithelial lymphocytes is found in the surface epithelium between the crypts. Although the normal range is between 5 and 100, the number of epithelial cells may be greater than 20 to 100. The mucosa that overlies the lymphoid nodules should be excluded during evaluation.
- The condition may involve crypts as well. A rare form of cryptal variant has also been described by the experts. Increased number of intraepithelial lymphocytes can be seen only in crypts and not on the surface epithelium.
- Surface mucosa is typically flattened with depleted mucin. Focal detachment can be observed with no overt ulceration.
- In around 38% of cases, occasional neutrophils can be found up to cryptitis. Common features include infrequent focal prominence with crypt abscesses with absence of inflammatory bowel disease and infection.
- Multinucleated giant cells that are located just below surface epithelial layer can be seen in some rare cases.
- No significant amount of crypt distortion is noticed. Mild crypt irregularity can be seen in around 4% of cases.
- Crypt distortion might be variably distributed within the colon. However, a single general biopsy does not rule out the disorder.
- Absence of any thickened layers of subepithelial collagen. There may be involvement of terminal ileum due to intramucosal lymphocytosis.
- Generally, normal levels are reported that shows 2 to 8 T cells or 100 enterocytes.
Lymphocytic Colitis Diagnosis
When trying to determine if an individual has lymphocytic colitis, the doctor will first evaluate the complete medical history of the patient and conduct a thorough physical examination. He will then ask questions regarding any medications that the patient might be taking, such as ibuprofen and aspirin, which may increase the risks of developing this disorder.
Among the tests conducted to confirm the diagnosis is a stool sample test, which might help to rule out the possibility of infection as a cause of persistent diarrhea. Blood tests are carried out to test for other abnormalities that may indicate lymphocytic colitis. Biopsies are performed from different areas of the patient’s colon during a colonoscopy or a sigmoidoscopy which may reveal abnormalities in the colon lining such as patchy distributions. Multiple biopsies are required to be taken from various regions of colon so that an accurate diagnosis can be made. The patchy appearance of the disorder is also the reason why Flexible sigmoidoscopy is often inadequate in the diagnosis of this condition as the abnormalities might not be detected in sigmoid colon in around 30%-40% of cases. This deficit is rectified by colonoscopy which allows the doctor to obtain biopsies of the other regions that are inaccessible by sigmoidoscopy.
Lymphocytic Colitis Differential Diagnosis
Lymphocytic colitis bears similarities to a lot of other health conditions in relation to their symptoms. Hence, a diagnostician needs to differentiate lymphocytic colitis from these conditions while confirming its presence. The differential diagnoses of the disease includes ensuring the absence of conditions like:
- Giardiasis
- Celiac sprue
- Diverticulosis
- Crohn’s disease
- Ulcerative colitis
- Hyperthyroidism
- Collagenous colitis
- Incidental Chronic Colitis
- Irritable bowel syndrome
- Autoimmune enteropathy
- Inflammatory Bowel Disease
Lymphocytic Colitis Treatment
Treatment for this condition may vary depending on symptoms as well as the severity of an individual case. The condition may resolve on its own without any treatment. However, treatment becomes necessary if the symptoms grow more serious. Doctors generally proceed stepwise while trying to cure this condition, and start with the simplest and easiest treatments. Certain lifestyle changes may be recommended to manage the condition. These might include following some dietary regulations and avoiding pain relievers like ibuprofen and aspirin. If these changes are not enough, a doctor can recommend the following medications:
Picture 2 – Lymphocytic colitis Image
Anti-diarrhea drugs
The medications that help in controlling diarrhea include bismuth subsalicylate (Pepto-Bismol), loperamide (Imodium A-D), as well as combination of atropine and diphenoxylate (Lomotil).
Steroid medications
These help in reducing inflammations. A corticosteroid drug like budesonide or prednisone can control inflammations of the colon.
Drugs that can block bile acids
Cholestyramine can absorb bile acids and reduce the diarrhetic symptoms.
Anti-inflammatory drugs
Medications like mesalamine (Pentasa, Asacol) and sulfasalazine (Azulfidine) can help to control colon inflammations.
Immunosuppressant drugs
These aid in reducing colon inflammation and include medications like azathioprine (Imuran, Azasan) and methotrexate (Rheumatrex).
If the symptoms of the disorder progress to a severe stage and medications are not effective enough, a doctor might recommend Colectomy – a surgical procedure in which all or a part of the colon is removed. Surgeries are rare for these disorders and should be opted for only when all other treatment methods have been tried out.
Lymphocytic Colitis Diet
Apart from taking the medications as prescribed by the doctor, the treatment of lymphocytic colitis also involves following a strict diet plan that will restore balance and create less pressure in the colon. An ideal diet plan for patients, which includes providing nutrition and making sure that the symptoms do not aggravate, is presented below:
- Low fiber foods like rice, mashed banana and potatoes are best to cure the symptoms of the colon. Although high fiber foods such as legumes, bran, oatmeal and barley are perfectly nutritious, they should be avoided when the colon is vulnerable. These foods may however be gradually added to the diet as there are noticeable changes in the condition of the colon and symptoms such as acidity, gas, diarrhea and abdominal cramps.
- Sometimes, patients might develop an aversion to dairy products. They might need to go to the restrooms after consuming some yogurt or a small amount of milk. These individuals have lactose intolerance and might develop rashes or severe diarrhea symptoms. Although patients do not always suffer from such lactose intolerance, they should stop consuming all dairy products if they feel they do so.
- A low-fat diet is best during these times. Excessive amounts of tea or caffeine as well as spicy or too much seasoned or fried foods should be avoided as well. The food items should be somewhat bland with little or no spices.
- Both freshly cut fruits and fruit juices are great ways to bring comfort to the colon. The daily intake of water should also be increased to at least 2 to 3 liters. This would help remove the toxins from the body.
Lymphocytic Colitis Complications
If left untreated, the disease may progress and result in any or all of the following complications:
- Weight loss
- Dehydration
- Malnutrition
- Malabsorption of the food nutrients
Lymphocytic Colitis Prognosis
The outcome of the disorder often depends on the severity of the symptoms. Nearly 20% of patients might experience spontaneous remission without any specific treatment. More than 50% of patients undergoing therapy have shown significant signs of improvement with reduced symptoms after only 6 months, whereas 15% of patients demonstrated signs and symptoms that were persistent. The symptoms of diarrhea may come and go over many years in certain patients. However, 80% or more patients have said that their symptoms of diarrhea along with histological abnormalities have resolved within 3 years. The condition does not result in colon cancer.
Lymphocytic colitis should be treated with medications and a proper diet plan to obtain optimum results.
References:
http://surgpathcriteria.stanford.edu/gi/lymphocytic-colitis/
http://www.mayoclinic.com/health/collagenous-colitis/DS00824
http://www.betterhealth.vic.gov.au/bhcv2/bhcarticles.nsf/pages/Collagenous_colitis
http://emedicine.medscape.com/article/180664-overview
The post Lymphocytic colitis appeared first on Prime Health Channel.
]]>