What is Ulcerative Colitis?
Page Contents
Ulcerative Colitis is a bowel disease that affects the colon or large intestine. It is also known as IBD (Inflammatory Bowel Disease) and incorporates a set of diseases affecting the gastrointestinal tract. It develops when the large intestine and rectum get inflamed resulting in tiny sores or ulcers on the colon lining. It starts in the rectum and spreads upwards involving the entire colon.
Inflammation induces bowel to move rapidly and discharge its contents quickly. Bowel lining has surface cells which die to form ulcers that release pus, mucus and also bleeding. It affects all ages, but mostly people between 15-35 age groups are diagnosed. UC have similar symptoms like irritable bowel syndrome and Crohn’s disease.
Difference between Ulcerative Colitis and Crohn’s disease
- Ulcerative Colitis: UC is limited to rectum and colon. It is a continuous pattern with intestine lining and inflammation. Patients can experience a relapse next year.
- Crohn’s disease: It can develop everywhere in GI tract between mouth and anus. It appears in patches that might extend through the thickness of the bowel wall. Patients will have minimum one relapse in next five years.
Causes
UC is a result of immune system failing to defend a bacteria or virus from inflaming intestinal walls. Other reasons are:
- Genetic: Risk increases if UC is prevalent in family history.
- Environmental Toxins: Single factor is not responsible for IBD and experts have detected viruses from tissue samples of patients.
- Psychological Factors: Stress might modify or worsen the disease.
- Immune System: Several changes contribute to the cause of IBD.
Symptoms
- Proctosigmoiditis: Inflammation in the sigmoid colon (lower end) and rectum along with abdominal cramps and pain, bloody diarrhea, urgency, rectal bleeding, etc.
- Ulcerative proctitis: Irritation only in the rectum with rectal bleeding. In severe conditions, rectal pains with a sudden urge to defecate, the panic of soiling, and painful bowel movement.
- Acute severe ulcerative colitis: Affects entire colon with profuse diarrhea, severe pain, fever, bleeding, etc.
- Left-sided colitis: Irritation expands from sigmoid to the rectum with signs like abdominal pain, weight loss, and bloody diarrhea.
- Pancolitis: Affecting the entire colon (left, right, transverse colon and rectum), it has rounds of severe bloody diarrhea, abdominal pain, weight loss, night sweats and fatigue.
- Fulminant Colitis: Rare and chronic type of pancolitis with severe dehydration, bloody diarrhea, abdominal cramps, and Patients can develop toxic megacolon and perforation (colon rupture).
Other Symptoms
- Soreness or Joint pain
- Anemia
- Appetite loss
- Sudden urge to go (especially at night)
- Feeling full (full colon) after using the bathroom
- Unable to hold stool
Symptoms get worse in the morning. However, it depends upon the bowel part affected.
Risk Factors
- Age: Usually seen before the age of 30, it affects men and women both.
- Race: It can occur in any race (specifically to the Ashkenazi Jewish descent, from Russia and Europe)
- Family History
- Accutane (Isotretinoin): Although it treats acne, it has been found to be the underlying cause.
Complications
- Bone loss
- Inflammation in eyes, joints and skin
- Colon cancer (Starts after 9-10 years of UC)
- Severe Bleeding (intestinal)
- Dehydration
- Perforated Colon
- Colon Swelling
- Liver disease
- Intestinal wall thickening
- Blood infection
- Kidney stones
- Blood clots in arteries and veins
- Erythema Nodosum (Painful red skin)
- Uveitis (Painful red eyes, also risk permanent vision loss)
Diagnosis
UC is confused with other diseases due to similar symptoms and multiple tests will help experts to diagnose. The tests include:
- Endoscopy: Flexible tube is used to examine small intestine, esophagus and
- Stool test: Stool is examined for parasites, blood, and
- Biopsy: Tissue sample is removed for examination from the colon and it allows knowing the intensity.
- CT scan: Particular X-ray for pelvis and abdomen
- Colonoscopy: Flexible tube is inserted to examine the rectum and visualize intestine. Colonoscopy allows direct visualization of the extension of colitis. Small tissues are also received during the process to check the severity.
- Blood tests: Complete blood count helps in detecting anemia, high sedimentation rate, C-reactive protein, kidney function, liver function, etc.
- Calprotectin: Responsive marker of the disease, it elevates before severe symptoms arise suggesting IBD. However, a single test cannot determine the condition.
- X-Ray: During the process, the liquid chalky substance is inserted into the rectum to inject the colon. Barium is dense and does not allow X-ray to pass through. Hence the outline is visible on X-ray images. However, it is inferiorly accurate than colonoscopy and direct visualization. If barium enema (X-ray) is done and UC is assumed, colonoscopy is essential for further diagnosis.
Treatments
- Diet Changes: Food is not a cause but can worsen the situation. It is advisable to eat snacks and meals that are high in protein and calorie, but low in fiber.
- Medicine: Antibiotics will help to fight infections and heal. Aminosalicylates lowers inflammation and reduces the symptoms. In most chronic cases corticosteroid is prescribed. For chronic ulcerative colitis, biologics drugs (made from living cells) are used.
- Surgery: Only used if other treatments don’t work. It involves the removal of the rectum and entire colon, operation eliminates the chances of developing cancer. However, surgery is not for all, and it is reserved for some specific patients who are not responding to medications and have toxic megacolon. Patients with high risk of developing colon cancers or are suffering from colitis for a more extended period have reacted poorly to medicines.
In a standard surgery entire colon is removed and a small opening is left open at the end of the small intestine that forms ileostomy. Stool gets collected in the bag attached to the ileostomy. With recent improvements continent ileostomy is created from intestine that acts like a rectum and it is emptied regularly with a tube.
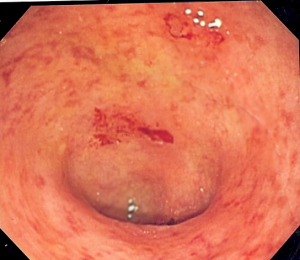
Pictures
Preventions
There is no evidence of what causes ulcerative colitis, but certain foods can worsen the situation. The following can help in preventing the disease to worsen:
- Minimize milk intake
- Avoid fatty foods
- Limit fiber-rich foods
- Eat small meals throughout the day
- Drink small amount of water throughout the day
- Avoid sodas (it will increase gas)