Are you suffering from a severe chest pain along with dizziness and shortness of breath? In that case, you might be having an aortic dissection. Read on to find out more about the causes, symptoms, diagnosis and treatment of this condition.
What is Aortic Dissection?
Page Contents
- 1 What is Aortic Dissection?
- 2 Aortic Dissection Classification
- 3 Aortic Dissection Causes and Risk Factors
- 4 Aortic Dissection Signs and Symptoms
- 5 Aortic Dissection Prevention
- 6 Aortic Dissection Diagnosis
- 7 Aortic Dissection Differential Diagnosis
- 8 Aortic Dissection Treatment
- 9 Aortic Dissection Complications
- 10 Aortic Dissection Follow-Up
- 11 Aortic Dissection Prognosis
- 12 Famous People affected by Aortic Dissection
- 13 Aortic Dissection Pictures
It is a condition that occurs when tearing in the inner layer or wall of aorta causes blood to flow or accumulate between the middle and inner layers of the aorta, causing the layers to grow apart. This new pathway for blood is referred to as “false lumen”. The dissection generally extends anterograde; however it can extend to a retrograde direction as well from the area of the intimal tearing.
The condition is also known as Dissecting Aneurysm.
Aortic Dissection Classification
Different methods of classification have been employed to analyze and describe dissections of the aorta. Methods that are commonly used to describe dissections either focus on the anatomy of the sufferer or the duration of beginning of symptoms before the presentation. At present, the Stanford Classification system is more prevalently used as it helps in the effective management of patients.
Stanford Classification System
This system divides aortic dissections into two groups, depending on the involvement of the ascending aorta.
A – Group A involves the ascending aorta, the aortic arch and possibly the descending aorta of a patient as well. The tear can take place in ascending aorta or aortic arch. In some rare cases, it can also originate in the descending aorta. Group A includes DeBakey types I, II as well as the retrograde type III.
B – Group B primarily involves descending aorta or aortic arch and does not involve the ascending aorta. It includes the DeBakey type III sans retrograde extension into ascending aorta.
DeBakey Classification System
It has been named after Michael E. DeBakey and includes an anatomical description of the dissection. It classifies dissections based on the location of the original intimal tear as well as the total extent of dissection.
Type I
It originates in the ascending aorta, then moves on to aortic arch and frequently beyond it distally. This is often considered to be the fatal form of the disorder.
Type II
It originates in the ascending aorta and remains confined to it.
Type III
This form originates in the descending aorta. It extends distally but is hardly likely to extend proximally. Type III frequently occurs in aged patients having hypertension and atherosclerosis.
Aortic Dissection Causes and Risk Factors
The various factors that might increase the risk of having this disorder include:
- Aging
- Atherosclerosis
- Blunt chest trauma
- High blood pressure
The other major health conditions and risk factors that are associated with development of Dissecting Aneurysm include the following:
- Pregnancy
- Turner syndrome
- Bicuspid aortic valve
- Ehlers-Danlos syndrome
- Connective tissue disorders
- Narrowing or coarctation of the aorta
- Marfan syndrome and other rare genetic disorders
- Heart surgery and other related cardiac procedures
- Swelling of blood vessels caused by conditions such as syphilis and arteritis
Aortic Dissection Signs and Symptoms
The symptoms of an acute case of this disease often vary from one patient to the other. Most patients generally complain of a sudden, intense pain in chest (thoracic aortic dissection), back or the abdomen (abdominal aortic dissection). Others may also experience:
- Shortness of breath
- Weakness
- Pain in the legs or arms
- Syncope (loss of consciousness)
Myocardial infarction or a heart attack may occur if dissections affect the arteries which supply the heart. If the blood supply to the patient’s brain is interrupted by dissection, he or she may experience a stroke.
Pain resulting from aortic dissection is often described as sharp, tearing, stabbing, or ripping. The pain may begin below chest bone and then move under shoulder blades or migrate to the back, neck, jaw, arms, abdomen, or the hips. The various symptoms e associated with Dissecting Aneurysm are listed below:
- Dizziness or faintness
- Shortness of breath
- Heavy sweating or clammy skin
- Vomiting and nausea
- Pallor or pale skin
- Rapid, weak pulse
- Orthopnea or difficulty in breathing while lying flat
- Stroke
- Abdominal pain
- Difficulty in swallowing, resulting from pressure on esophagus
- A feeling of impending doom
- Congestive heart failure
- Weaker pulse in one of the arms
- Sudden difficulty in speaking
- Loss of vision
Apart from the above mentioned symptoms, occlusion of the smaller arteries may also cause the following conditions:
- Angina
- Paraplegia
- Limb ischaemia
- Neurological deficiency
Aortic Dissection Prevention
Conditions such as atherosclerosis and high blood pressure should be properly treated which can reduce the risk of aortic dissection. Safety measures must be taken to avoid injuries that may cause aortic dissection. Many aortic dissection cases cannot be prevented. In case a patient has been diagnosed with Marfan or Ehlers-Danlos Syndrome, he or she should visit the doctor regularly for checkups.
Aortic Dissection Diagnosis
The proper diagnosis of Dissecting Aneurysm is often difficult as its symptoms are often similar to a variety of other conditions. Although a doctor takes into consideration the medical history as well as the physical signs and symptoms of a patient, the diagnosis of dissection is difficult based on history or physical signs alone. A doctor may choose to inspect the intimal flap by conducting a diagnostic imaging examination. Diagnosis is also done by conducting a trans-esophageal echocardiogram and a Computerized Tomography scan of chest using iodinated contrast material. Other tests which may be helpful in diagnosis may comprise of an aortogram or a magnetic resonance angiogram (MRA) of aorta. The tests have got their own advantages and disadvantages and do not have the equal sensitivity and specificity in diagnosing Dissecting Aneurysm. The imaging technique that is chosen depends on the availability of testing modality, pre-test likelihood of diagnosis, patient stability as well as specificity and sensitivity of the test.
Some of the main diagnostic tests for this condition may include the following:
- Chest MRI
- Aortogram
- Blood tests
- Chest X-Ray
- D-Dimer Test
- Echocardiogram
- Aortic angiography
- Doppler Ultrasonography
- Magnetic resonance angiogram
- Transesophageal echocardiogram
- Computerized Tomography scan of the chest using dye
Aortic Dissection Differential Diagnosis
During diagnosis, a doctor should also look out for many other conditions which are similar in appearance or symptoms. The differential diagnosis for Dissecting Aneurysm includes distinguishing its symptoms from those of the following conditions:
- Pleuritis
- Pericarditis
- Cholecystitis
- Mediastinal tumors
- Pulmonary embolism
- Musculoskeletal pain
- Aortic aneurysms without any dissection
- Aortic regurgitation without any dissection
- Cholesterol or atherosclerotic embolism
- Acute coronary syndrome both with and without any ST-elevation
Aortic Dissection Treatment
For acute cases, the treatment depends on the location of the rupture. In case of Stanford Type A ascending Dissecting Aneurysm, surgical management of the dissection is more important than medical management. For the Stanford Type B distal aortic dissections and abdominal aortic dissections, the doctor prefers to use medical management over surgical management.
The possibility of death due to Dissecting Aneurysm is the maximum during the first couple of hours after the onset of the dissection and then gradually decreases afterwards. Due to this, the treatment procedures for acute cases of the disease are different from that of its chronic cases. In case of a Dissecting Aneurysm, an individual presents the symptoms within the initial 2 weeks. If he or she survives during this period, there is an improvement in his or her prognosis. Nearly two-thirds of all cases of this type of dissection fall in the acute category. Patients who present symptoms 2 weeks after the beginning of dissection suffer from chronic Dissecting Aneurysms, and can be treated medically as long as their conditions are stable.
Medications
Dissecting Aneurysm is considered to be a case of hypertensive emergency, with the main priority of medical management being strict control of blood pressure. The blood pressure should be kept at a range between 60 mmHg to 75 mmHg which comprises the mean arterial pressure or MAP. It can also be kept at the lowest level of blood pressure that a patient can tolerate. The shear-force of blood ejection from left ventricle should also be reduced.
Patients of acute and chronic cases of Dissecting Aneurysm are firstly treated with beta blockers. Acute dissection patients are given titratable parenteral agents like:
- Esmolol
- Propranolol
- Labetalol
Hypertension sufferers can be treated with vasodilators like sodium nitroprusside. However, they should not be used alone because they can cause reflex tachycardia.
A doctor may also use calcium channel blockers like diltiazem and verapamil on finding signs of contraindication to beta blockers.
Surgical procedures
Surgery is used for treatment of acute proximal aortic dissections and acute distal aortic dissections with one or additional complications. The complications might include:
- Damage of an important organ
- Rupture of the aorta
- A history of Ehlers-Danlos Syndrome or Marfan syndrome
- Retrograde dissection into ascending aorta
The main objective of surgical management of dissection is the removal of the most significantly damaged portions of the aorta as well as to stop entry of blood in the false lumen. Although a doctor might perform excision of intimal tear, it does not change mortality in a significant way.
The various methods of repairing aortic dissection include the following:
- Use of David procedure, which involves replacement of damaged portion of aorta as well as re-implantation of aortic valve.
- Use of Bentall procedure, which involves replacement of damaged portion of aorta as well as replacement of aortic valve.
- Replacing the damaged portion of the aorta with tube graft, when the aortic valve is not damaged.
- Insertion of a stent graft in TEVAR (Thoracic Endovascular Aortic Repair).
- Replacing the damaged portion of the aorta by a sutureless vascular ring connector-reinforced dacron graft.
Aortic Dissection Complications
Dissecting Aneurysm is considered to be a major medical emergency and it can lead to a quick death, even after optimal treatment. Rapid and massive blood loss takes place if the dissection completely tears open the aorta through all the 3 layers.
Complications from Dissecting Aneurysm depend on the site of the tearing as well as the extent of the condition. Dissection may lead to the occlusion of the aortic branches that can cause damage to the supplied organs. Occlusion may be of the kidney (renal), spinal, iliac or the coronary arteries. There may be rupture of false lumen in the aorta, or in the pericardium or mediastinum.
Associated complications of Aortic Dissection include the following conditions:
- Myocardial infarction
- Aortic diastolic murmur
- Aortic regurgitation
- Cardiac failure
- Hypotension
- Syncope
- Superior vena cava obstruction
- Increase levels of lactate dehydrogenase and acute phase proteins
Aortic Dissection Follow-Up
Long-term follow up of patients, who survive the symptoms of Dissecting Aneurysm, include strict monitoring of the blood pressure. The risk of a late rupture of aortic aneurysm is ten times higher in patients having uncontrolled hypertension. The risk of death is highest in first 2 years after the initial event. During this time, patients should be monitored closely. 29% of the late-deaths occurring after surgery are caused by rupture of dissecting aneurysm or some other form of aneurysm. A new aneurysm may also be formed by the dilatation of residual false lumen.
Aortic Dissection Prognosis
There is a high risk of death for untreated patients of this condition. Dissections that result in rupture have a mortality rate of 80% associated to them, of which 50% patients die even before they are brought to the hospital. Although the risk of death is very high during the first 24 hours, most of the patients who survive this initial stage have a much better chance of survival. 75% of untreated patients die within the first two weeks. Survivors are required to be treated throughout life for high blood pressure. Regular CT scans should be conducted to monitor the condition of the aorta.
Famous People affected by Aortic Dissection
Some renowned personalities who have suffered from this condition are:
- John Ritter
- Dr. Michael E. DeBakey
- Lucille Ball
- Gérard Houllier
- Lux Interior
- Liese Prokop
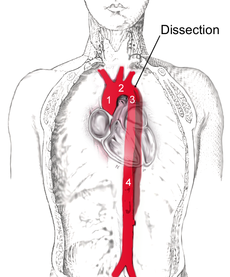
Aortic Dissection Pictures
Here are some pictures that reveal the conditions associated with this disorder.
Picture 1 – Aortic dissection
Picture 2 – Aortic dissection Image
Aortic dissection is an emergency condition that can lead to severe internal injury, pain and even death. Immediate medical attention is required for helping the patient survive, after which more long term treatment may be conducted.
References:
http://www.cdemcurriculum.org/ssm/cardiovascular/cv_tad.php
http://en.wikipedia.org/wiki/Aortic_dissection
http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001233/
http://www.medicinenet.com/aortic_dissection/page4.htm#how_is_aortic_dissection_diagnosed