Marasmus is a serious condition that reportedly affects over 50 million children in the Third World countries who are less than 5 years of age. Read and know all about the causes, symptoms, diagnosis and treatment of this dreaded disease.
What is Marasmus?
Page Contents
It is a form of malnutrition that arises most commonly in infants in the developing countries who are less than one year of age. It is an extreme type of emaciation and wasting resulting due to lack of protein and energy in the body.
The word “marasmus” is also used to make an approximate reference to “Anaclitic Depression.” It is a term coined by René Spitz to denote all those children who suffer from the loss of their mother in the very early stages of their life without getting a proper substitute.
Marasmus Incidence
The disease is most common in kids living in developing regions like South Asia, Latin America and Africa where poor and unhygienic conditions contribute to the cause. Marasmus, along with Kwashiorkor and Cachexia, belong to a group of disorders that are collectively known as PEM (Protein-energy malnutrition). As per a study conducted by the WHO (World Health Organization), 49% of the deaths of 10.4 million children under five in developing nations occur due to PEM (protein energy malnutrition).
Marasmus Symptoms
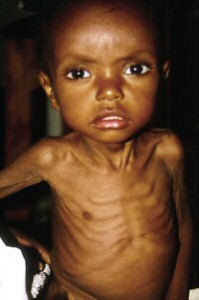
The condition is mainly characterized by reduced weight gain. The rate of weight gain is lower than that of increase in height which creates a mismatch. Consequently, the head of affected children appear quite large than the rest of their body.
One of the most distinct features of this disorder is a progressive wasting of muscle and subcutaneous fat of the body. Due to this, there is a rapid decrease in the amount of body fat which makes the skin appear quite loose and the bones more prominent. Patients generally suffer from lethargy as their bodies attempt to conserve energy. Extreme hunger and irritability are two of the most common signs of wasting. Acute wasting for a prolonged duration may lead to permanent retardation.
Some of the other obvious effects of this condition include:
- Chronic diarrhea
- Delayed healing of wounds
- Distended or flat abdomen
- Hypotonia
- Abnormal limbs
- Subnormal body temperature
- Impaired immunity
- Increased appetite
- Vomiting
- Listlessness
- Muscle atrophy
- No hepatic enlargement or edema
- Progressive weight loss, resulting in emaciation in severe cases
- Sunken eyes
- Shrill and weak cry
Marasmus Causes
The condition primarily results from a lack of essential nutrients, particularly protein, in the human body. Protein consists of polymers of amino acids which are important for the growth of animals as well as for the repair of tissues. The disease also arises due to an inability to digest nutrients properly. Both causes can result in malnutrition, a problem where the body does not receive enough protein and calories essential for its functioning and growth. Malnutrition, which is one of the most serious types of PEM in the world, can range from an inadequacy of some vitamins to complete starvation.
Maramus is commonly caused when an infant undergoes a transition from breast milk to other foods. As is known, breast milk is a wholesome food for babies and supplies them with all the essential nutrients needed for their survival and growth. Women often stop breastfeeding due to various reasons, which range from social pressure to an inability to develop milk. If breast milk is not followed up with a similar wholesome diet, Maramus can arise as a consequence.
The condition may also be caused due to acute and chronic infections, particularly in case of children who are already susceptible as a result of borderline malnutrition.
Some of the other major causes of this disease are:
- Early loss of mother, resulting in lactation failure without any alternative means for breastfeeding
- Long-term starvation as a part of medical treatment for diarrhea
- Lack of food
- Infective diarrhea, caused by the use of unsterilized feeding bottles
This condition, if allowed to persist, can turn very serious. It can get acute enough to resist treatment. It can become impossible to cure patients. This usually happens as the body of sufferers become incapable of absorbing nutrients as a result of physical damage caused by malnutrition.
Marasmus Diagnosis
A physical examination is typically enough to diagnose this condition. Further medical tests are not required unless doctors wish to detect particular complications or monitor treatment. In such cases, laboratory tests for the condition may involve:
Blood Glucose Analysis
If the level of blood glucose is <3 mmol/L, it may indicate the presence of Hypoglycemia.
Direct Detection Test or Microscopy
It involves examination of blood smears to check for presence of parasites. If tests are positive, doctors can confirm an infection.
Urine examination and culture
An infection can be indicated if there are over 10 leukocytes per high-power field.
Albumin test
If albumin level is found to be less than 35 g/L, it can indicate massive impairment of protein synthesis. This is not useful as a diagnostic test and is, rather, helpful for prognosis.
HIV test
It is not to be used as a routine examination. If carried out, it should be followed by counseling the parents of sufferers. The results should be kept confidential.
Marasmus Treatment
Treatment of this disease involves using a specific feeding and rehydration plan for the patient. The health of the sufferer should also be closely observed to avoid or manage complications arising due to malnutrition.
The various modes for treatment of Marasmus include:
Well-balanced diet
A well-balanced diet rich in nutrients and plenty of fresh fruits, grains, vegetables and protein can help lower the risk of malnutrition and any associated ailments, such as Marasmus.
Vitamin B5 restoration
Vitamin B5 deficiency, associated to the condition, can be compensated by vitamin supplements.
Herbs
Asian herbs like Ashwgandha, Bala, Guduchi, Shatavari and Vidnaga can be administered in 1 gram dose along with milk and water to improve the digestive capacity and overall health of patients. Western herbs, such as Marshmallow, Ginseng and Fo-ti are also useful. Taking in 1 teaspoon of chyavanprasha 3 times a day can also show improvement after a month.
Oil massage
Regular massage with Vata palliating oils duch as Dhanvantari, Narayan and Bala, can improve digestive power in patients and increase their appetite. It is considered to be the best treatment for improving the digestive capability.
Sun exposure
Exposure to early morning sun every day for 15 minutes can also help boost health.
Nasogastric feeding tubes, Oral rehydration solutions and Intravenous fluids are other forms of treatment that may be used for cure. In some regions and countries, pediatric nutrition rehabilitation centers have been set up to organize treatment of children suffering from malnourishment.
Marasmus Complications
In infants as well as young children, there are serious complications associated with malnutrition or Marasmus. Inadequate nutrition can result in retarded physical and mental development of patients. Some of the most serious complications of untreated Marasmus may include:
- Loss of strength
- Growth problems
- Deformity and destruction of joints
- Loss of vision, which can ultimately lead to blindness
- Organ dysfunction or failure
- Unconsciousness
- Coma
Some of the complications may result in permanent or long-term Sequelae and give rise to developmental issues. In case of early massive iron deficiency anemia and extensive impairment of growth, patients may suffer from permanently retarded mental and physical development. Evidently, the younger the patient is at the time of malnourishment, the more devastating the long-term effects are to be. In extreme cases, lack of treatment can even result in the death of a patient.
Marasmus Prognosis
If proper treatment and follow-up care is adopted, the prognosis can be good even in case of severe Marasmus. Generally, the outcome is seen to be better than in patients of Kwashiorkor which in another PEM disorder.
Once medical treatment begins, the weight of patients should be monitored after every fortnight. This can help determine whether the mode of treatment is proper and should be continued.
Marasmus Prevention
It is important to prevent Diarrhea to avoid this condition. The treatment options for Marasmus are greatly effective. However, they do not last long until healthy practices are implemented in a consistent manner.
Some of the general measures that can be used to prevent Marasmus include:
Following a well-balanced diet
A good, well-balanced diet comprising of the essential minerals and vitamins can help prevent most disorders related with malnutrition. A diet comprising of foods rich in protein, such as skimmed milk, fish and eggs, can supply kids with enough energy for activities and growth. Vegetables and fruits can restore the deficiencies caused by vitamins and minerals. It is essential to add solid foods slowly and over a period of time to avoid adverse complications arising due to poor digestive capability of sufferers.
Cooking foods at a high heat
It is essential to cook foods to a high temperature while preparing them. This will help destroy the bacteria present in them and help avoid cases of infections.
Store foods in a clean place
It is also important to store foods in a freezer so as to prevent the development of bacteria. Food items that are kept refrigerated should be heated again before consumption in future. All utensils should be thoroughly cleaned before keeping foods in them. Cross-contamination between various foods should always be avoided.
In developing nations, it is also important to educate mothers about the benefits of breastfeeding and advice them to feed children with breast milk for as long as they can.
Marasmus vs Kwashiokar
Kids who suffer from marasmus are typically younger than those affected by Kwashiokar. Marasmic Children typically look skinnier whereas kids affected with Kwashiokar have swollen limbs. Unlike Kwashiokar patients, marasmic infants do not suffer from acute vision problems or liver ailments. It is also easier to treat a marasmic child than one suffering from Kwashiokar. However, hospitalization is required in severe cases of both the conditions. Antibiotic treatment may also be required if the disease is accompanied by infections. A Kwashiokar child is considered to be sicker than a marasmic child with a higher mortality rate due to the more complex deficiencies that they suffer from. Children with kwashiokar fail to efficiently digest fat in the body.
Senile Marasmus
It is a term used for the disorder famously known as Anorexia. In the Italian language, however, this term was used to describe senility as well as loss of all superior functions due to old-age. The condition can be managed and prevented from worsening with the aid of brain exercises that stimulate the frontal lobe, which controls attention, memory, decision-making, sense of humor and other faculties. In a recently conducted research, such exercises were conducted on three thousand elderly patients. Within a few days after performance, the brain functions began to be active again. Proper low-fat nutrition and regular physical exercises can also help keep the brain young and functional. According to some experts, making love and solving crosswords can also be beneficial to manage this problem.
Marasmus Pictures
Take a look at these Marasmus images to know how infants suffering from this condition look like. The Marasmus photos collected here will help you get an exact idea about the physical symptoms produced by this disorder.
If your child is showing retarded physical development or any other symptoms of this condition, immediately get in touch with a professional medical care provider. Timely diagnosis and proper medical treatment can help cure many disorders and fortunately, Marasmus is one of them.
References:
http://www.bettermedicine.com/article/marasmus
http://emedicine.medscape.com/article/984496-overview
http://www.rightdiagnosis.com/m/marasmus/intro.htm
http://www.healblog.net/medical/marasmus-causes-signs-and-symptoms-treatment/