The post Subungual Melanoma appeared first on Prime Health Channel.
]]>Melanoma is a kind of skin cancer that begins to grow in the cells comprising of skin pigments called melanocytes. When melanocytes start to collect, it results in the formation of moles that may turn cancerous. In case Melanoma is not treated timely, cancer might spread to other organs. Melanoma usually occurs when an individual is exposed to the ultraviolet rays of the sun.
What is Subungual Melanoma?
Subungual Melanoma is a rare condition of Melanoma under the fingernails. Unlike other skin cancers, it occurs on the nail bed, known as the nail matrix, which helps in protecting the underlying skin. It causes the nail to discolor and is characterized by dark brown or purple color appearing as a streak of dark pigmentation that results in thinning and ultimately breakage of the nail. It is often seen on the big toe or thumbnail. However, it may occur in any nail of the foot or hand.
Subungual Melanoma Incidence
It is noted that 1% – 5% of all melanoma cases are of Subungual Melanoma affecting the fingernails of both males and females. It is most common in Asians and those of the African-American descent who are intensely pigmented. It is largely found in people within the age group of 60-70 years. It is however rarely seen in children. This form usually is non-malignant but if cancerous can prove harmful leading even to death.
Appearance of Subungual Melanoma
Although in a few cases, the nail might not face pigmentation, the early symptom is a streak of pigmentation on the nail bed. It is quite visible to the naked eye. During its development through the days, it appears like:
- Pigment turns first into light brown, purple or black
- Gradually spreads out and covers the closest nail fold
- Tends to become wider on the cuticle
Symptoms of Subungual Melanoma
In most cases, a dark patch appears underneath the nail. Many females may not be able to see the initial signs if they wear dark shades of nail paints. In its early development, it looks like a mole on the skin which is caused by the sun rays.
- Small lump under the nail without any color
- Dark purple, black or brown spot on the nail
- Blood from the nails but no pain
- Streak or band of light to dark brown color on the nail mostly vertical
- Dark brown or purple band tends to expand and slowly grow
- Pigmentation may also extend to the skin surrounding the nail
- Nodule underneath the nail with or without a pigmentation band
- Affected nail appears cracked, thin and brittle
- Bleeding along with the pigmentation
- Patches or the streaks on the nails
- Bruise on the nail that does not heal soon
- Nails of the finger or toes get separated from the nail bed
- Skin adhering to the nail gets darkened
- Nodule develops underneath the nail causing bleeding
- Nail bed gets distorted
- Split nails
- Painless bleeding of the cells in the nails
Causes of Subungual Melanoma
Primarily the reason for this disorder is cancer. Mainly three categories of cancer urge the occurrence of Subungal Melanoma-
- Acral lentiginous melanoma affects the nail matrix
- Desmoplastic Melanoma.
- Nodular melanoma.
Diagnosis of Subungal Melanoma
Diagnosing this form of cancer is difficult which is why it is highly recommended to consult a doctor immediately after noticing any patch or any unusual growth on the nails. The doctor needs to examine the region of the nail and the lesion carefully. Dermatologists may use an instrument called a dermascope which helps them to get a magnified view of the affected nail and its surrounding area.
But in a few cases, visual inspection may be harmful as it may be confused with other disorders like the subungual hematoma, onychomycosis.
The only technique for detection is a biopsy. Two procedures are:
- A biopsy is known as a punch biopsy is a tubular instrument containing a sharp end that acts like a cookie cutter that collects the sample. It enables the doctor to look for other fungal infections apart from melanoma.
- For advanced melanoma suspicion, the biopsy associated with the excision is undergone to remove the entire part of the nail along with its surrounding tissue.
Risk factors regarding Subungal Melanoma
People who prone to get affected by risk factors do not immediately get affected by this disease. But they bear the risk of suffering more than the ordinary ones. Hence they should be more careful with the early symptoms and readily visit a doctor.
Some of the common risk factors include:
- Exposure to direct sun and ultraviolet rays light for a prolonged period
- People having darker skin are more likely to suffer
- People aged above 50 are more at risk
- Medical history associated with trauma to the fingers or toes increases the risk
- Patients affected by HIV or other immunosuppressive disorders
- Genetic history of melanoma
- Occurrence of several moles
- Hereditary conditions of Xeroderma Pigmentosa (extreme sensitivity to UV radiation)
Complications caused by Subungal Melanoma
Similar to other cancers if not treated timely it can spread to other parts of the body. Melanoma affects other organs causing life risks. At times, the doctor may suggest an amputation to be done on the finger or the toe on which the nail gets pigmented. However, compared to this, surgery is more advisable.
Treatment for Subungal Melanoma
The preferred method to get rid of Subungal Melanoma is to adopt a surgery. The doctor firstly removes the entire nail affected and then it can help him to discard the cancer development thoroughly. But again, this depends on the intensity of the disorder verifying on what stage it is and how complicated can it get.
- Initially, if the depth is less than one millimeter, then the doctor usually undergoes local expurgation. It can help to control the development of cancer.
- In case, it is wider and dangerous, an excision is required along with the biopsy of the lymph node. It is needed to conduct the nature of the melanoma and reduce the risk of spreading to other organs through medications and proper methods.
- But if the melanoma is too advanced, then the affected finger or toe needs to be operated and removed. Thus all of the cancerous element presents can be expurgated entirely and thereby no further complications can arise.
- Unfortunately, if the surgery does not work, then the last option is to undergo chemotherapy and use of prescribed medicines to kill cancer in the cells of the affected area or anywhere surrounding it.
However, till date, the most viable option for the cure of this melanoma is surgery.
Pictures of Subungual Melanoma
The post Subungual Melanoma appeared first on Prime Health Channel.
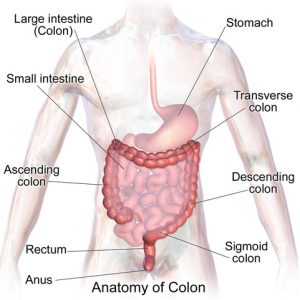
]]>The post Inflamed Colon appeared first on Prime Health Channel.
]]>Inflamed colon known as Colitis in medical terms is a disorder caused in the intestines (both large & small intestines) that cause abnormalities and bowel diseases.
Types of Inflamed Colon
Crohn’s disease
A part of the gastrointestinal tract gets inflamed by this type of colitis. The tail end of the small intestine is mostly affected, but it can affect all the layers of the bowel. It causes inflammation and creates patches across different parts of the digestive tract.
Ulcerative colitis
It acutely affects the large intestine causing the lining of the colon to develop ulcers and sores that excrete pus and mucus at times. It causes inflammation in the intestine and abdominal discomfort. It also causes a continuous inflammation in one particular area and results to affect deeper into the intestine.
Diverticulitis
It occurs when the outer lining of the bowel pouches out through the layers of the spots present in the muscles of the intestinal wall. As a result of this, inflammation or infection is caused in the digestive tract. The small pores face obstruction from parts of stool and other infectious materials. The nearest tissue of the colon present on the left-hand side is inflamed and thereby causes pain and even fever. However, this can be treated by antibiotics. If not treated through medication, the condition worsens further leading to leakage of the colon and moreover blockage of the bowel. In that case, surgery is a must to remove the affected area of the intestine.
Antibiotic-Associated Colitis
The colon usually consists of natural and healthy bacteria. Intake of antibiotics for treatment of any disease might kill these useful bacteria thereby allowing the other harmful bacteria to affect the colon causing inflammation. The most common type is named Clostridium difficile and it generates the disease called antibiotic-associated colitis. In case it is mild, it may be healed by taking metronidazole orally. In moderate cases, it can be treated by vancomycin which is also taken orally. But in acute conditions, the patient should be medicated with a mixture of oral vancomycin and metronidazole generated through a vein and vancomycin enemas. But when it comes to more severe issues such as bowel rupture, surgery is advised. Again, some complicated cases of this disease can be overcome by fecal pellets donated to the patient.
Chemical Colitis
When chemicals get inserted into the colon, the colon gets inflamed, and major damages can occur. The mucosal lining of the colon might also get inflamed when reacted to strong chemicals.
Medication-associated colitis
Inflamed colon can also be the effect of intake of several medicines such as NSAIDs (nonsteroidal anti-inflammatory drugs), mycophenolate, ipilimumab and retinoic acid.
Causes of Inflamed Colon
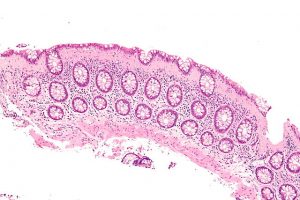
Collagenous colitis intermed mag (Inflamed colon)
Colitis tends to occur more in younger people than the aged ones. The major causes are as follows:
- Bacteria: One of the vital causes, most of these enter the human body through food and causes disorders, food poisoning or other stomach infections.
- Parasite infections: A significant cause of infectious colitis, it mainly occurs due to contamination of water. Infected water causes serious issues.
- Pseudomembranous colitis: Mainly caused by a specific bacterial infection known as Clostridium. People taking antibiotics or admitted at the hospitals tend to suffer from this kind of colitis. Most antibiotics kill the good bacteria and replace them with the Clostridium bacteria causing diarrhea along with fever.
- Lack of Supply of Blood: Arteries which supply blood to the colon sometimes tend to narrow themselves. As a result, the required amount of blood fails to enter the colon causing inflammation. Lack of blood supply in the human body can cause abnormal bowel movements containing blood, abdominal pain and also fever.
Symptoms of Inflamed Colon
- Fever sometimes accompanied with chills
- Frequent bowel movements
- Loss of appetite
- Considerable weight loss
- Diarrhea (sometimes with the presence of blood)
- Abdominal pain or cramps
- Feeling tired and restless
- Constipation
- Muscular spasms
- Deficiency of iron
Diagnosis of Colitis
Some tests and diagnostic methods are to be carried out, they include:
- Blood test
- Stool test
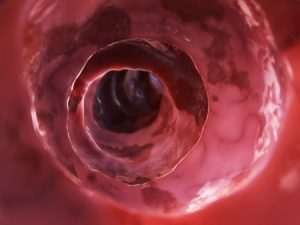
- Colonoscopy (endoscopy using camera to provide the entire view of the colon and the surrounding part)
- Biopsy should be undergone to collect a small sample of the tissue for diagnosis
- Video capsule endoscopy
- CT scan
- Special X-ray named small bowel fellow
- Enterography is done to find out if there is inflammation
Treatments for colitis
There is no immediate treatment for this, and the general procedure is to lessen the signs and symptoms. Doctors may suggest a drug therapy, and if not cured, the ultimate step is to undergo surgery. A few mild medicines may be prescribed.
Some common drugs that are used to reduce the symptoms are as follows:
- Antibiotics (prescribed to control the disease and prevent it from spreading)
- Anti-inflammatory drugs (usually used to prevent the inflammation)
- Immunosuppressant (Helps to prevent further irritation in the colon)
Natural home remedies
- Have smaller meals at intervals throughout the day at least five to six times
- Taking multivitamins and minerals can help as inflamed colon causes a lack of nutrients
- Smoking should be avoided to minimize the risk of inflammation
- Limit stressful situation and reduce mental stress by simple exercising to reduce depression
- Yoga and meditation might also help
Recommended foods to reduce Colitis
- Drink enough amounts of fluids as the body gets dehydrated during diarrhea
- Include probiotics like cheese and yogurt in your diet
- Soluble fiber foods, barley, grains and peeled fruits are equally helpful
Foods to Avoid
- Prefer steamed or boiled vegetables instead of eating them raw
- Fruits like berries and pineapples
- Avoid having whole grains such as oatmeal, nuts or seeds
- Avoid eating cooked greens like cabbages or corn
- While having meats try to stew them and make it softer
- Avoid alcoholic drinks too, instead drink lots of water and sports’ drinks
- Stay away from spicy foods which can irritate the bowel movement
- Tea, coffee, dairy products and even chocolate is a strictly a no-no
Prevention of Inflamed Colon
- Primary reasons are the inadequate supply of proper and clean drinking water, unhygienic sanitation leading to affect thousands of people even causing death. Also in the developed nations, poor conditions of hand washing and kitchen hygiene bring in infectious colitis. So the primary way to prevent it is to maintain cleanliness everywhere.
- On the other hand, inflammatory bowel disorders might be problematic to deal with as they are hereditary. It also generates an abnormal auto-immune response to an unidentified stimulus in the body.
- Ischemic colitis occurs when the blood vessels connecting to the bowel begin to narrow. This condition lowers the risk for other types of circulatory disorders like peripheral vascular disease, heart attack and even resulting in a stroke. The primary reasons are smoking habits, high blood pressure, high levels of cholesterol and diabetic tendency too.
When to visit a doctor?
If any of the following symptoms arise, a doctor must immediately be informed:
- Temperature above 101°F or fever along with chills
- Stools containing blood most of the times
- Lightheadedness, rapid heart rate or frequent passing out
- Frequent vomiting
- Severe abdominal pain at times with bloating.
- Acute dehydration causing minimum or no urine for almost 12 hours or more
- Secretion of pus from around the anus
- Pain and swelling in the anal area
- No excretion of stools
The post Inflamed Colon appeared first on Prime Health Channel.
]]>The post Burkitt’s Lymphoma appeared first on Prime Health Channel.
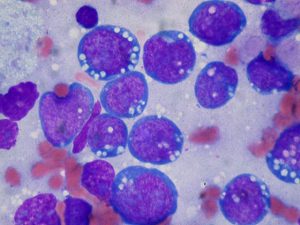
]]>Burkitt’s lymphoma (BL), also called Burkitt lymphoma, Burkitt’s tumor, or malignant lymphoma, is a rare cancer of the lymphatic system, particularly of the B cells, accounting for about 0.3% to 1.3% of all non-Hodgkin lymphomas. The condition is named after British surgeon Denis Burkitt, who discovered the disease in African children and young adults. Considered to be the fastest growing tumors affecting humans, it may spread to various parts of the body.
What Causes Burkitt’s Lymphoma
Impaired Immunity: It is often associated with a weak immune system, with the condition often detected in African children suffering from Malaria. It is believed that BL occurs when malaria weakens the immune system’s reaction towards the Epstein-Barr virus (responsible for nasopharyngeal lymphoma, glandular fever and mononucleosis), such that the infected B cells are converted to cancerous cells. The mode of transmission of EBV is usually through saliva.
Genetic Factors: It may have some other causative factors apart from an impaired immune system, like chromosomal translocation involving chromosome 8, which may alter the mode of expression of the gene, c‑Myc, thereby disrupting its normal function. This can lead to an unrestrained growth of B lymphocytes, resulting in the cancerous disorder.
What are the Types of Burkitt’s Lymphoma
The condition can be classified into three types:
- Endemic (African): Always associated with chronic malaria and EBV infection, it can affect the gastrointestinal tract, ovaries, breasts and central nervous system.
- Sporadic (Non African): May or may not be associated with EBV infection, and often involves the liver, colon spleen, bone marrow, brain or spinal fluid.
- Immunodeficiency Related: Usually associated with the intake of immunosuppressive drugs, such as those used for preventing organ transplant rejection or treating HIV and AIDS.
Risk Factors: Who is Likely to Have BL
- Young boys between 5 and 8 years of age
- Although rare in adults, males are more at risk
- People with a weak immune system like those infected with HIV/AIDS
- Those living in regions of North Africa, South America, the Middle East and Papua New Guinea
Signs and Symptoms
Common Symptoms
- Fever
- Loss of weight
- Night sweats
- Distortion of bones of the face
- Loss of appetite
Endemic BL
A swollen lymph node is one of the earliest symptoms of this type of BL. Swelling of lymph nodes in the chest or neck may lead to:
- Sore throat
- Swallowing difficulty
Another endemic symptom involving the oral cavity comprises of fast growing tumors of the jaw (mandible), or some other facial bone that have a doubling time of 24 hours. It mostly occurs in children.
Sporadic and Immunodeficiency Related BL
- Pain in the abdomen
- Feeling of a heavy, abdominal mass
- Enlarged tonsils
The condition may spread to other body parts, leading to characteristic symptoms.
Related to the GI Tract
- Diarrhea
- Nausea
Related to the Central Nervous System
- Headache
- Seizures
- Mental confusion
- Paralysis
Related to the Bone Marrow
- Shortness of breath and weakness suggesting anemia
- Bleeding from bowel or any other bruise indicating low platelet count
Complications
- Intestinal obstruction
- Tumour lysis syndrome
- Peripheral neuropathy
- Leukaemic transformation
Diagnosis and Tests
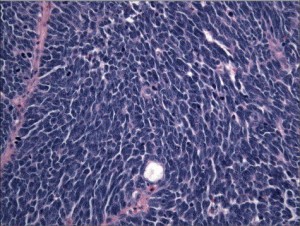
Since the symptoms have a sudden onset, early diagnosis is required. After a physical examination, a biopsy of all or a portion of a swelled lymph node or other suspicious regions is done to confirm the disease. A microscopic view of the affected tissue reveals a “starry sky” appearance, typical of the condition.
http://www.ganfyd.org/images/9/93/Burkitt_lymphoma_starry_sky_1.jpg
Burkitt’s Lymphoma Starry Sky Appearance
Other relevant tests may involve:
- Computed tomographic (CT) imaging of certain body parts such as the chest, pelvis, abdomen to find out the concerned lymph nodes and organs
- Examination of bone marrow and spinal fluid
- X-ray of the chest
- MRI scan or PET scan
- An ECG or MUGA scan to check if the heart is working properly or not
- A 24-hour urine collection to determine kidney function
- Blood tests to find out liver function
- Tests to detect HIV infection
- Peripheral blood smear
Differential Diagnosis
- Lymphoblastic lymphoma
- Blastic mantle cell lymphoma
- Diffuse large B-cell lymphoma
- Prolymphocytic SLL/CLL
BL Staging
Different stages of the condition that depend on the location and nature of the swollen lymph nodes as well as organ involvements are:
Stage 1: Lymphoma occurring either above or below the diaphragm, but is restricted to a single group of lymph nodes only
Stage 2: Lymphoma occurring in either two or more locations on the same side of the diaphragm
Stage 3: Lymphoma occurring on both sides of the diaphragm
Stage 4: Lymphoma found in bone marrow or central nervous system
Treatment and Management
Intensive Intravenous Chemotherapy
This is often the preferred treatment with a high success rate since it may successfully destroy most of the lymphoma cells.
Intrathecal Chemotherapy
Also called CNS prophylaxis, this is carried out by injecting the chemotherapy drugs directly into the spinal fluid, since the condition may spread to the fluid that surrounds the brain and spinal cord. The drugs that are used in various combinations include cyclophosphamide (Cytoxan), doxorubicin (Adriamycin), cytarabine (Cytosar-U, Tarabine PFS), and methotrexate (Rheumatrex).
Intrathecal chemotherapy is at times used in combination with other treatments such as:
- Treatment with a monoclonal antibody called, rituximab (Rituxan), which gets attached to a protein CD20 present on the surface of cancerous B cells, that stimulates the immune system to destroy the damaged cells.
- Transplantation of stem cells, carried out by removing, storing and returning stem cells to the body of the diseased individual
- Radiation therapy
- Steroid therapy
Surgery
In the case of intestinal obstruction, surgery is carried out.
New Treatments for BL
According to the findings of a new clinical trial, treatment with low-intensity chemotherapy may increase the survival rate of adult patients having BL.
Treatment of Associated Conditions
- Mesna and folinic acid to help combat the side effects induced by the chemotherapy drugs
- Administration of rasburicase (Fasturtec) initially, and later allopurinol (Zyloprim) to provide protection against tumor lysis syndrome
- Anti-sickness drugs (antiemetics)
- Prophylactic (preventive) antibiotics and antifungals, to reduce infection risks
- Growth factors (G-CSF), so that there is a fast recovery of the bone marrow
Follow-up Treatment
A patient is required to have monthly checkups after chemotherapy to detect if the lymphoma is relapsing or not. The rate of such checkups is decreased, if, at the end of six months, lymphoma does not recur. However, there can be long term side effects like reduced fertility and heart ailments.
Prognosis and Survival Rates
The outcome generally depends on the stage of BL at the time of diagnosis as well as the age of the patient. If the cancer has not spread, the survival rate is as high as 90% for both adults and children. However, the outlook for elderly patients is usually poor. The condition rarely occurs during pregnancy, but has a poor outcome when it does.
BL Prevention
Though there are no known ways to prevent BL, certain lifestyle modifications such as reducing HIV infection risks in relation to the sporadic form, may aid in reducing the possibility of having the disease. The condition may also be handled naturally by maintaining a healthy diet consisting of sprouts, and green vegetables.
Incidence and Prevalence
Sporadic BL is rare in developed countries; about 1200 people in the US are diagnosed with the condition each year. Endemic BL, on the other hand, has a high incidence in Africa, accounting for about one-half of childhood cancers.
Burkitt’s lymphoma ICD‑9‑CM and ICD‑10 Codes
The ICD‑9‑CM code of Burkitt’s lymphoma is 200.2, and the ICD‑10 code is C83.7.
The post Burkitt’s Lymphoma appeared first on Prime Health Channel.
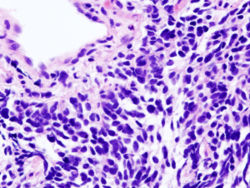
]]>The post T-cell Lymphoma appeared first on Prime Health Channel.
]]>T cell Lymphoma (TCL) is one of the four kinds of lymphoma that affect T-cells, the small lymphocytes that develop in the thymus. These can be related with Human T-cell leukemia virus-1 or Epstein Barr virus.
T-cell Lymphoma Incidence
The condition accounts for 8% of all cases of cancer involving same classes of blood cells. 2% of these cases are cutaneous T cell lymphomas and 2% are precursor T lymphoblastic.
T-cell Lymphoma Classification
The condition can be differentiated into a number of subtypes on the basis of their size, shape and other characteristics of the tumor cells. The classification of these tumors is complicated in nature as the majority of the tumors are different from other neoplasms.
TCL can generally be classified into the following categories:
Peripheral T cell Lymphoma
It is a very rare type of T cell Lymphoma that arises in mature T-cells. The condition is more common in grown-ups than in children. This is an aggressive, high-grade form of cancer.
Cutaneous T cell Lymphoma (CTCL)
It is a rare, low-grade form of Non-Hodgkin’s Lymphoma. This type of cancer has a slow progression and primarily affects the white blood cells known as T-cells in the skin.
Angioimmunoblastic T cell lymphoma (AILT)
Also referred to as Immunoblastic lymphadenopathy, it is a type of aggressive cancer that develops in the T-cells. It accounts for 1% of all cases of Non-Hodgkin’s Lymphomas (NHL) and is mostly found to affect the elderly population.
Hepatosplenic lymphoma (HSTCL)
It affects the T lymphocytes in the lymphatic system and is more specifically referred to as Hepatosplenic T cell lymphoma. It is not necessarily common for sufferers to have enlarged or inflamed lymph nodes, unlike many other types of Lymphomas.
Adult T cell Lymphoma (ATLL or ATL)
It is also referred to as adult T cell leukemia or HTLV-1 and is regarded as a Peripheral T cell lymphoma (PTCL). The condition is very rare in the U.S although it is reported to be more common in Japan and other regions of Asia.
This form of TCL is aggressive in nature and is further categorized into the following four subtypes:
- Acute ATL
- Lymphocytic ATL
- Chronic ATL
- Smouldering ATL
The first two subtypes are quite aggressive in nature and the last two are slow-growing. The Human Lymphotropic Virus-1 (HTVL-1) is responsible for this disorder.
The HTVL-1 virus is present in certain ethnic populations such as Caribbean, South America and Japan. However, only 2-5% of all infected individuals develop the disorder.
T-cell Lymphoma Symptoms
The signs and symptoms of this condition can vary on the basis of the location and stage of malignancy in the body. It can often be difficult to distinguish these symptoms from those of common ailments like flu or cold.
Some of the common signs of this disorder involve:
- Fever
- Headaches
- Unexplained weight loss
- Skin rash or itchy skin (Pruritus)
- Coughing or shortness of breath
- Difficulty moving parts of the body
- Night sweats that often soak the sheets
- Persistent fatigue, lethargy, feeling of tiredness
- Pain in the chest, abdomen or bones for no apparent cause
- Inflammation in the lymph nodes in the neck, underarms, groin, or abdomen
Due to the similarity of the symptoms with those of common disorders, it is essential for patients to get in touch with expert medical professionals who can carry out an accurate diagnosis.
T-cell Lymphoma Causes
It is not known what exactly results in the development of the majority of cases of TCL. However, it is possible that genetic alterations occurring at the time of antigen processing and presentation leads to an aggressively dividing cell population that may cause TCL.
T-cell Lymphoma Risk Factors
There are no known risk factors for this condition as TCL is found to arise mainly as a result of genetic changes. However, Adult TCL is found to arise more in people of the Asian regions. Due to this reason, being of Asian origin is supposed to increase the susceptibility of a person to Adult TCL.
T-cell Lymphoma Diagnosis
Lymphomas can develop from the lymph nodes that are located all over the body and are named according to the tissue where they originate. Due to this reason, a T cell lymphoma can be definitely diagnosed by an evaluation of cell types that are present in biopsy samples of tissue. This diagnostic process is contrary to another form of lymphoma, like a B-cell lymphoma.
The detection of TCL is usually based on the type of the condition that one suffers from:
Diagnosis of Peripheral TCL
A biopsy can be used for detecting PTCL in humans. Physicians can also look for physical signs associated with the development of the condition.
Diagnosis of Cutaneous TCL
It is diagnosed with the aid of biopsy which involves removal of a small part of the affected tissue for laboratory analysis. In the majority of cases of CTCL, the process is comparatively simple and can be performed with local anesthetics.
Diagnosis of Angioimmunoblastic TCL
This type of TCL can be detected with the help of a lymph node biopsy as well as other follow-up exams such as PET scans, x-rays, bone marrow biopsies and CT scans for staging of the disorder. Concrete information about staging is not available due to the rarity of the condition.
Diagnosis of Adult TCL
Biopsies are generally useful for the detection of this form of TCL.
Diagnosis of Hepatosplenic Lymphoma (HSTCL)
A bone marrow biopsy of the condition is likely to yield positive outcomes, as the involvement of bone marrow is common. Meanwhile, blood tests may reveal low blood counts or certain evidence of Cytopenia.
T-cell Lymphoma Differential Diagnosis
The differential diagnosis of TCL involves distinguishing the signs of the condition from those of similar disorders, such as:
- Allergic Contact Dermatitis
- Autoimmune lymphoproliferative syndrome (ALPS)
- Angiofollicular lymphoid hyperplasia (Castleman disease)
- Granulomatous disease
- Irritant Contact Dermatitis
- Lichen Planus
- Parapsoriasis
- Pediatric Atopic Dermatitis
- Pemphigus Foliaceus
- Plaque Psoriasis
- Pustular Psoriasis
- Tinea Corporis
- Paracortical (T zone) lymphoid hyperplasaia
- Kikuchi-Fujimoto disease, proliferative phase
- Paracortical (T zone) lymphoid hyperplasia
- Sézary syndrome (SS)
- T large granular lymphocytic leukemia
- T-cell prolymphocytic leukaemia (T-PLL)
T-cell Lymphoma Treatment
The treatment of TCL depends on the type of the disorder that a person suffers from.
Peripheral T cell Lymphoma Treatment
The treatment options for PTCL include steroids, chemotherapy, bone marrow transplant and radiotherapy. However, there is no gold-standard cure for recurring PTCL.
Cutaneous T cell Lymphoma Treatment
There are numerous treatment options for the disorder. The choice of treatment generally depends on the stage of the condition. The curative options that are usually opted for include:
- Photopheresis
- UVB Therapy
- PUVA treatment
- Topical treatment options
- Radiation
- Chemotherapy
- Bexarotene capsules
Angioimmunoblastic T cell lymphoma Treatment
The treatment for the disease generally begins with steroids that can help cure rashes and inflammation. The CHOP regimen of chemotherapy is generally administered after steroid treatment. Bone marrow transplants are generally tried in cases of recurrence of Adult TCL.
Adult T cell Lymphoma Treatment
An allogenic transplant may offer some amount of hope to approximately 40% of sufferers. IFN-alpha therapy or Zidovudine has been a little effectual in patients likely to show poor outcome. However, the treatment for this form of the disease has yet to be proven on a broader scale.
Hepatosplenic lymphoma Treatment
Combination chemotherapy tends to be the preferred curative option for people detected with this condition. In this process, one of the drugs to be administered is most likely to belong to the anthracycline class like Doxorubicin. However, medical treatment is not considered to be widely successful and recurrences are highly common, as is the case with many other forms of TCL.
HSTCL is a refractory and aggressive disorder. Due to this reason, it is difficult to treat. The median period of survival for patients from the time of diagnosis is said to be approximately 3 years.
T-cell Lymphoma Prognosis
The outcome of the condition depends on a variety of factors, such as the age of patients and the stage of the disorder. Those under the age of 60 and having a good performance status, stage 1 or 2 cancer and limited or non-existent lymph node involvement have a better prognosis. Those over 60 years of age, suffering from stage 3 or 4 cancer, poor PS, high LH levels and involvement of multiple lymph nodes show a poor outcome.
T-cell Lymphoma Survival Rate
Around 75% people in the lowest risk-group and only 30% of individuals in the highest risk-group have a 5 year survival rate.
T-cell Lymphoma Complications
The complications commonly associated with this condition include:
- Anemia or other blood abnormalities
- Enlargement of liver or spleen
- Malignancy
Death may also occur in older patients and in case of involvement of more than one lymph node. The survival rate is low in such people. Prompt treatment can ensure somewhat lower risk of life-threatening complications although that is often not true in case of aged patients.
T-cell Lymphoma Prevention
There is no known way to prevent this disease. However, its rapid progression and associated complications can be prevented by consulting a qualified medical professional on an earlier basis and undergoing diagnosis and treatment as early as possible.
T-cell Lymphoma in Dogs
TCL, along with B-cell Lymphoma, is one of the two types of lymphoma cancers that may affect dogs. TCL in dogs is referred to as Canine lymphosarcoma and generally arises in the bone marrow or the lymphatic system. Eventually, it spreads to the other regions of the body if left untreated. Suffering dogs may experience symptoms like inflamed lymph node, weight loss, fever, vomiting and weakness. Microscopic analysis of biopsy sample is usually the definitive diagnostic procedure for TCL in dogs. Intravenous chemotherapy is the most effective curative option for Canine lymphosarcoma.
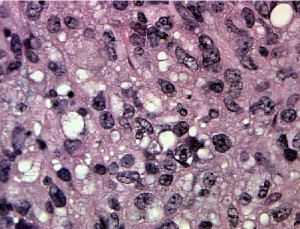
T-cell Lymphoma Pictures
The following images will help you get an idea about the physical appearance of those suffering from TCL.
Picture 1 – T-cell Lymphoma
Picture 2 – T-cell Lymphoma Image
If you suspect yourself or a family member to be suffering from any form of TCL, do not delay treatment. Get in touch with a doctor as soon as possible and get tested. Faster detection and treatment has been found to reduce the risk of progression and improve the outcome for sufferers.
References:
http://www.cancercenter.com/non-hodgkin-lymphoma/t-cell-lymphoma.cfm
http://www.lymphomainfo.net/nhl/t-cell.html
http://en.wikipedia.org/wiki/T-cell_lymphoma
http://www.wisegeek.com/what-is-t-cell-lymphoma.htm
The post T-cell Lymphoma appeared first on Prime Health Channel.
]]>The post Seminoma appeared first on Prime Health Channel.
]]>Seminoma Definition
It is one of the two major forms of cancer of the testicles, the male reproductive glands that are positioned in the scrotum. It is a slow-growing tumor that is generally found in men who are between 30-40 years of age. Generally, the cancer is only in the testicles although it may spread to the lymph nodes.
This tumor is also referred to as “Classical Seminoma” or “Pure Seminoma”.
Seminoma ICD9 Code
The ICD9 Code for this disorder is 186.
Seminoma Epidemiology
The overall incidence of this type of tumor is 6-10 times higher in white people than black ones, which is demonstrated in all age groups. It is interesting to note that the overall development of GCT, and particularly Seminoma, has an important relation with people of high economic status.
For reasons unknown, the overall incidence of this type of humor has progressively increased in various different countries in the 21st century.
Seminoma Types
Seminoma is unilateral, or affects only one of the testicles of patients. It is of two types:
Benign
This type of lump is generally benign, or non-cancerous in nature. This testicular lump is not progressive or recurrent.
Malignant
It arises only in rare cases. As the name indicates, this form of lump is cancerous.
Seminoma Causes
These tumors are known to be associated with:
- Some intersex syndromes
- A family history or previous history of Testicular GCT
- Cryptorchidism
- Oligospermic infertility
Some other factors, that have also considered to be related with Seminoma, involve:
- Exposure to organochlorine
- Being subjected to Chemotherapy or Radiotherapy
- High levels of estrogen
- Marijuana abuse
- Testicular microlithiasis
- Nutrition status at the time of infancy
However, the above factors have not been confirmed to be actually associated with this disease.
In the recent decades, genetic association has also been evaluated. In around 80% of Seminomas, a consistent change in chromosome is present.
Seminoma Symptoms
The mean age of manifestation of symptoms is 40 years. In patients of nonseminomatous testicular tumors, this median age is around 30 to 35 years. Seminoma tumors can also arise in older men. In rare cases, it may also be found to develop in younger boys.
In general, Seminomas do not result in any signs and symptoms and are detected when men observe lumps in their testicles. Up to 90% of affected individuals manifest symptoms such as inflammation or other palpable abnormalities. In rare cases, sufferers may also experience pain.
Locationwise, the majority of Seminoma tumors are intratesticular. These develop in the germ cells in the testicles. These can arise in extragonadal regions along the midline of the human body. Typical extragonadal spots include the Central Nervous System (CNS) and the mediastinum.
Variations in behavior and medical outcome indicate that Seminomas in the mediastinal spots are biologically different from those in gonadal spots. In contrast, tumors that develop in the retroperitoneum are almost always related with premalignant lesions in one of the testicles. Clinically, these can behave like metastatic testicular Seminomas.
Increased levels of the serum hCG or human chorionic gonadotropin may occur in Seminomas. These may correlate with syncytriotrophoblastic giant cells, as may be seen histologically. Serum hcG has a mild to moderate increase in around 10% sufferers of clinical Stage I Seminoma as well as 25% people with metastasis. Even in that case, Gynecomastia is rare.
Alpha fetoprotein (AFP) is not produced by cells of Seminoma. The detection of its serum generally suggests a nonseminomatous component. However, minimal elevations of AFP may be as a result of Hepatopathy, including Metastatic Seminoma to the liver.
Seminoma Risk Factors
The strongest risk factor for this disease is Cryptorchidism, with an increase in risk as much for the contralateral one as for the affected testis. Cryptorchidism is a fetal abnormality that arises when one or both testes are unable to descend into the scrotum from the region of their development in the abdomen.
Those with a history of testicular cancer or undescended testicles are at a higher risk of developing malignant tumors such as Seminoma.
Other factors include:
- HIV infection
- Abnormal development of testicles
- Being of Asian-American or African-American origin
- Having Klinefelter Syndrome
While men in their 30s or 40s are most susceptible to this type of tumor, these growths can arise at any age.
Seminoma Diagnosis
Testicular self exams are suggested for men, to let them spot the changes that indicate tumors as well as other health problems. In cases where a lump is detected, medical assessment can involve:
- Bloodwork, to detect the levels of certain hormones (as some hormones can increase or decrease due to testicular cancers)
- Medical imaging exams of the testicle
The results and findings obtained through such tests can help physicians develop a proper diagnostic and treatment plan.
Seminoma Treatment
This form of cancer shows very good response to medical treatment, particularly when detected in the early stages. The outcome for sufferers can be excellent if they get proper treatment in time.
Hitorically, the preferred treatment for this condition has been the removal of the testicle that is affected. According to medical studies, there is no need for surgical removal of testicles when Seminoma is caught in the early stages. Chemotherapy or radiation can be equally effective. Such growths are extremely susceptible to chemotherapy and radiation treatment measures and should shrink after a number of sessions. Testicle removal can be explored as a curable option in case there is a concern regarding reduced response to medical treatment.
Treatment and management of these growths are essentially the same, whether patients are 15 or 50 years of age. Both oncologists and urologists can be involved in the treatment of this type of cancer, aided by supportive care providers such as nurses. If there are concerns about future fertility, one can consult a fertility specialist to receive additional information.
These growths have a very slow growth. They can spread to the lymph nodes as well as other areas of the body if they are not timely detected. Due to this reason, physicians usually recommend medical imaging studies for men with Seminoma to detect signs of malignant cells elsewhere in the body.
Seminoma Complications
The possible complications of this disorder include:
Metastasis
The cancer commonly spreads to other areas of the body, such as the lungs, spine, abdomen and retroperitoneal region – the area close to the kidneys behind the other organs in the abdominal area.
Post-operative problems
There can be complications of surgery, such as infection and bleeding in the post-operative stages. If both testicles are removed, problems of infertility would arise.
Seminoma Prognosis
This is one of the most curable forms of cancer. For men with early-stage Seminoma, the survival rate is higher than 95%. Based on the size of the tumor and the time of initiation of treatment, the disease-free rate of survival for Stage II and III cancers is a little reduced.
Seminoma Prevention
The risk of development of this condition can be lowered by carefully monitoring the health of sufferers. Those having a family history of the disease, or similar conditions, should make appointment with physicians in case of any abnormal changes. This can ensure early diagnosis and treatment for cancers.
As no effective screening technique is known, The United States Preventive Services has recommended against routine screening for cancer of the testicles. However, the recommendation is not applicable if there is a personal history of an undescended testis.
Seminoma Support Groups
Patients of this condition often suffer from ailment-related stress by joining a support group. Visit http://www.cancer.org for support and further information. This is the official website for The National Cancer Institute.
Seminoma in Dogs
This is the second most common form of testicular tumor in male dogs. It typically affects dogs older than 4 years.
Causes
The condition is supposed to arise as a result of the fetal abnormality known as Cryptorchidism.
Appearance and Symptoms
The diameter of these growths usually measure less than 2 cms. In affected dogs, no clinical symptoms are manifested in Seminoma. Due to this reason, these growths are difficult to detect. Some dogs, however, suffer from pain as a result of pressure from the enlarging tumor. The testicular tumor in dogs can be felt in a few cases. In still rarer cases, some growths of this type can turn malignant and metastasize to other areas of the body.
Diagnosis
The condition is diagnosed in dogs by a physical examination, conducted by veterinarians. During physical tests, vets usually look for a testicular lump and try to ascertain whether or not they are palpable. Dogs with these types of growths may suffer from pain and abnormally large testicles.
Generally, laboratory tests like CBC (Complete Blood Count), Urinalysis and biochemistry profile are within normal ranges. However, an ultrasound examination of the testicular tissue may show the presence of a lump.
In cases where an abnormal lump is revealed, a veterinarian may perform a biopsy of a tissue of the testicular lump for further assessment. If that is not possible, affected dogs may require castration for confirmation of the diagnosis.
Treatment
The preferred choice of treatment is the removal of tumor, which can best be done by castration of the affected dog. However, if the tumor is malignant or has metastasized to other areas of the body, chemotherapy may be recommended by veterinarians.
Prognosis
Usually, the overall outcome is excellent for affected dogs that undergo castration. However, this depends on whether or not the tumor is malignant or benign.
Seminoma Pictures
The images below would help you understand how this abnormal testicular lump looks like.
Picture 1 – Seminoma
Picture 2 – Seminoma Image
If you suspect yourself or anyone in your family, such as your pets, to be suffering from Seminomas, make an immediate appointment with a professional health care provider to get an earlier diagnosis and treatment. As aforesaid, this condition can be cured and prevented from worsening with the aid of quicker detection and cure. Naturally, you should not delay curative options while the disorder is still in its early stages.
References:
http://emedicine.medscape.com/article/437966-overview
http://www.wisegeek.com/what-is-a-seminoma.htm
http://www.nlm.nih.gov/medlineplus/ency/article/001288.htm
http://www.petmd.com/dog/conditions/reproductive/c_dg_seminoma
The post Seminoma appeared first on Prime Health Channel.
]]>The post Small cell lung cancer appeared first on Prime Health Channel.
]]>Small cell lung cancer Definition
SCLC is the name given to a form of lung cancer that has a fast progression. It spreads in a much faster manner than NSCLC (Non- small cell lung cancer).
SCLC accounts for about 20-25% of all forms of lung cancer.
Small cell lung cancer Types
SCLC is classified into the following two types:
- Small cell carcinoma (also referred to as Oat Cell Cancer)
- Combined Small cell carcinoma
The majority of SCLCs are of the first form.
Small cell lung cancer Incidence
Lung cancer is responsible for the death of around 160,000 individuals in the U.S every year. SCLC accounts for 15% of all cases of lung cancer. Males are slightly more prone to this disorder than females.
Small cell lung cancer Symptoms
This is the most aggressive type of lung cancer. It generally arises in the bronchi (breathing tubes) in the middle of the chest. The cancer cells, although small in size, grow very fast and give rise to large tumors. These tumors often metastasize very quickly to other regions of the body, including the bone, liver and brain.
The signs and symptoms of this type of cancer include:
- Fever
- Difficulty in swallowing
- Weakness
- Hoarseness or changing voice
- Facial swelling
- Bloody sputum (phlegm)
- Loss of appetite
- Weight loss
- Chest pain
- Cough
- Wheezing
- Shortness of breath
The majority of signs and symptoms of SCLC do not arise until after the development of a tumor in the lungs. These tumors give rise to symptoms such as breathing and coughing. In some cases, patients are even found to cough up blood. In more severe cases, where the cancer is found to spread to other regions of the body, symptoms might involve:
- Difficulties in swallowing
- Hoarse voice
- Headaches
- Back pain
Small cell lung cancer Causes
Nearly all cases of this condition occur as a result of smoking cigarettes. It is rare in people who have never smoked in life. SCLC is often associated with distinct paraneoplastic syndromes, a collection of symptoms that arise from substances manufactured by the tumor.
Small cell lung cancer Risk Factors
The risk factors for this disorder include the following:
Smoking
Active or passive smoking of cigarettes is the major risk factor for this disorder. According to one particular study, smoking of cigarettes has been associated with bigger tumors than non-smoking during the time of presentation.
Being aged
Cancerous conditions of the lungs are also associated with advanced age.
Cancer history
Those with an earlier history of cancer, particularly those of neck and head, are also more susceptible to lung cancers.
Having COPD
Individuals with Chronic Obstructive Pulmonary Disease (COPD) are also more prone to SCLC.
Industrial dust diseases
Exposure to industrial dusts such as arsenic, chromium, asbestos and iron oxides can give rise to industrial dust disorders and make a person more susceptible to SCLC. Exposure to asbestos is said to increase the risk of lung cancer by 9 times. A combination of cigarette smoking and asbestos exposure increases the risk of SCLC by as much as 50 times. The risk of SCLC is most common in individuals who mine Uranium.
Small cell lung cancer Diagnosis
The diagnosis of this disorder begins with a physical examination of patients and asking them about their medical history. Patients are enquired whether or not they smoke, and if they do – the amount and duration of their smoking are also taken into account.
During physical examination, doctors listen to the chest with the aid of a stethoscope. At the time of this exam, they can sometimes hear sounds produced by the fluid around the lungs or the regions where the lungs suffers a partial collapse. Each of these results can indicate cancer, although that is not always the case.
By the time of diagnosis, SCLC usually spreads to other sections of the body of sufferers.
The diagnostic exams used for the detection of this condition involve the following:
- Chest x-ray
- MRI scan
- CT scan
- Liver function tests
- Complete Blood Count (CBC)
- Bone scan
- Sputum test (detection of cancerous cells, Cytology)
- Positron Emission Tomography scan (PET scan)
- Thoracentesis (removal of fluid from the chest cavity surrounding the lungs)
In some cases, the areas where cancer is found to spread are noticed as large tumors on imaging tests such as x-rays. Early on, however, these regions may not be visible although they may still be there.
The common lab tests for this disease include testing of samples of urine, blood and other substances in the body. These exams can help diagnose the disorder, develop treatment plan and monitor the condition over a period of time.
In the majority of cases, doctors may require removal of a tissue sample from the lungs or other regions to examine it under a microscope. This is known as a Biopsy, a common process that can be done in various ways:
- Open lung biopsy
- Pleural biopsy
- Mediastinoscopy with biopsy
- Video-assisted thoracoscopy
- CT scan-directed needle biopsy
- Bronchoscopy, along with biopsy
- Endoscopic esophageal ultrasound (EUS) with biopsy
Generally, if a biopsy reveals the presence of cancer, further imaging exams are performed to determine the stage of the cancer. Based on the size of the tumor and how far it has spread, SCLC is classified into either of the following two types:
Limited SCLC
In this form, the cancer is only in one side of the chest and can be cured with the aid of radiation therapy. It involves only one section of the lung and adjoining lymph nodes.
Extensive SCLC
In this form, cancer is found to have spread in the region outside the chest.
Small cell lung cancer Differential Diagnosis
The differential diagnosis of SCLC involves distinguishing its signs and symptoms from those of other disorders that give rise to similar problems. These include:
- Lung Adenoma
- Lung Hamartoma Imaging
- Mediastinal Lymphoma
- Non-Small Cell Lung Cancer
- Atypical Carcinoid Lung Tumor
- Large Cell Neuroendocrine Carcinoma
Physicians should make sure that patients are not suffering from any of the aforementioned conditions and the symptoms that they are experiencing are those of SCLC only.
Small cell lung cancer Treatment
As this cancerous condition quickly spreads all through the body, its treatment must involve oral administration or injection of chemotherapy medications. Generally, the chemotherapy medicine known as Etoposide (or Irinotecan in some cases) is combined with either Carboplatin or Cisplatin.
A combination of radiation treatment and chemotherapy is given to individuals in whom SCLC has spread all through the body. However, this type of treatment only helps to alleviate the symptoms and not cure the disease itself.
Radiation therapy makes use of powerful x-rays or other types of radiation to destroy cancerous cells. If surgery is impossible, radiation therapy can be used in combination with chemotherapy. The aim of radiation therapy may be any of the following:
- Curing the underlying cancer, along with chemotherapy, if it is not possible to perform surgery
- Aiding in providing relief from the pain caused by cancer that has spread to the bones
- Aiding in providing relief from the symptoms resulting from cancer, such as inflammation and breathing problems
Often, the cancer may have already spread to the brain even in the absence of any symptoms or other cancerous signs in the brain. Due to this reason, radiation therapy may be administered to certain patients with smaller cancers or those who showed a positive response in the first round of chemotherapy. This procedure is referred to as Prophylactic cranial irradiation (PCI).
Very few SCLC sufferers are aided by surgery as the disease is found to have often metastasized by the time it is detected. Operation may be carried out when there is only a single tumor that has not spread. If surgery is performed, radiation therapy or chemotherapy will be required still.
Small cell lung cancer Prognosis
The outcome of the condition depends on the extent of spread of this form of lung cancer. This form of cancer is extremely life-threatening. Only around 6% of all SCLC patients manage to survive even 5 years after detection.
Some factors affect the outcome as well as treatment options for this condition. These include:
- Age of patients
- Gender of patients
- General health of patients
- The stage of the cancer, whether it is restricted to the chest cavity or has spread to other regions of the body
Small cell lung cancer Life Expectancy
If the malignancy is checked in the initial stages, the five year survival-rate is found to be only 20%. Patients generally live for less than one year once cancer enters an advanced stage. The earlier the condition is diagnosed and treated, the better the chances of survival are. The disorder shows a good response to chemotherapy and radiation therapy.
Unfortunately, for all advances in medicine, there has been little change in life expectancy associated with this condition for the last two decades. This is true for both the limited as well as the extensive form of SCLC.
Small cell lung cancer Complications
The complications of SCLC involve the following:
- Side effects of other operation, radiation therapy or chemotherapy
- Metastasis of cancer (spreading of cancer to other regions of the body)
Small cell lung cancer Prevention
As the disorder is found to arise mainly as a result of smoking, it is wise to give up smoking. Those who do not smoke should avoid the company of smokers to prevent secondhand smoke or passive smoke. In high-risk populations, lung-cancer screening programs should be used. Those engaged in industrial professions should avoid occupational exposure to carcinogens.
Coping with Small cell lung cancer
Numerous studies indicate that acquiring more information about lung cancer can improve the quality of life and possibly even the outcome of the disorder. Patients would do better to learn about clinical trials for this disease. Clinical trials, at present, are in progress for both stages of SCLC. These help in evaluating new treat options and curative combinations for this form of aggressive cancer. According to NCI (National Cancer Institute), everyone with SCLC may be considered for involvement in clinical trials.
Small cell lung cancer Support Group
SCLC patients and their friends or family members can get in touch with the various support groups that exist to provide guidance and information to sufferers of this disorder.
American Cancer Society
Official Website – http://www.cancer.org
Cancer Care
National Cancer Institute
Small cell lung cancer Pictures
The following images demonstrate the appearance of cancerous lung cells in SCLC patients.
Picture 1 – Small cell lung cancer
Picture 2 – Small cell lung cancer Image
If you suspect yourself to be suffering from signs of Small cell lung cancer, get in touch with a healthcare provider as fast as you can. This is particularly important if you are a smoker. Early treatment can check the malignant condition at its early stage and increase your chances of making a complete and faster recovery from this disorder.
References:
http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001180/
http://www.emedicinehealth.com/small-cell_lung_cancer/article_em.htm
http://www.wisegeek.net/what-is-small-cell-lung-cancer.htm
http://www.webmd.com/lung-cancer/guide/small-cell-lung-cancer
The post Small cell lung cancer appeared first on Prime Health Channel.
]]>The post Ewing’s Sarcoma appeared first on Prime Health Channel.
]]>Ewing Sarcoma, or Ewing’s Sarcoma, is a type of primary bone cancer that is commonly seen in children and teenagers. The cancerous cells are mainly found in the bones and soft tissues. The tumors generally occur in the femur, the pelvis, the humerus, the clavicle and the ribs.
It is included in the cancer group named Ewing Sarcoma Family of Tumors (ESFT) along with primitive neuroectodermal tumors because both these conditions are usually associated with a common genetic locus. Otherwise, the two diseases are completely different.
This disorder has been named after American pathologist James Ewing who was the first person to describe the tumor. He established it as a separate condition from other cancers like lymphoma.
Ewing Sarcoma Stages
The condition has two primary stages:
Localized tumor
Ewing’s Sarcoma is considered to be a localized condition when it involves only the nearby tissues like the muscles and tendons. The condition is considered to be localized only if the diagnostic studies do not detect the tumor to affect distant organs.
Metastatic tumor
The metastatic stage denotes that the tumor has already spread to various other organs and body parts from its original location. In these cases, the tumor can affect other bones and their bone marrow as well as organs like the lungs, liver, kidney and lymph nodes.
Ewing Sarcoma Causes
The causes behind the development of this cancer are not clearly known. Like many other forms of tumors, it is known to result mainly due to the abnormal growth of certain stem cells which gradually forms the tumor.
Ewing Sarcoma and Genetics
Researchers have shown chromosomal changes in the DNA of a cell to be a possible cause of the disorder. These changes develop in a child after birth instead of being inherited. But the reasons for these changes are not evident.
Certain cells may become cancerous due to genetic exchange between some chromosomes. Translocation between the chromosome 11 and chromosome 12 causes most (85%) of the Ewing’s Sarcoma cases. The EWS gene located on chromosome 22 gets fused with the FLI1 gene located on chromosome 11 due to this translocation.
Ewing Sarcoma Symptoms
The condition can lead to various signs and symptoms depending on the size and location of the tumor. The common symptoms include:
- Pain around the area of the tumor
- Redness and/or swelling around the area of tumor
- Decreased appetite
- Fever
- Weight loss
- Fatigue
- Loss of bladder and bowel control (in cases where the tumor is located in the spine)
- Symptoms associated with nerve compression due to the tumor (including tingling, numbness and paralysis)
A growing tumor can put extreme pressure on the bones and soft tissues around it. This considerably weakens the bones, increasing the risk of bone fractures in a patient.
Ewing Sarcoma Prevention
It is not possible to prevent the disorder because of its unclear etiology. The risk factors responsible for triggering the genetic changes are not known to be associated with any environmental elements or even radiation exposure.
Ewing Sarcoma Diagnosis
Pain and swelling in the legs, arms, back, chest and trunk are the initial symptoms. The condition often goes undiagnosed until it leads to more serious symptoms. In many cases, the disorder is first suspected after the bone weakness becomes evident as the bones break easily after small injuries.
Imaging Tests
Various imaging studies are used for diagnosing this disorder. During these tests, the patients may be given contrast dye injections or asked to drink contrast solutions to develop clear images. These imaging tests include:
X-ray
X-ray images are useful for observing the internal bone structures to detect any abnormality around them. It is very useful for diagnosing the tumors.
CT (Computerized Tomography) scan
A CT scan helps to create cross-sectional images of the bones and soft tissues by combining the x-ray findings. This helps to detect the tumors.
MRI (Magnetic resonance imaging)
This diagnostic procedure is used for producing detailed images of the bones in the affected area. The MRI can help the doctor to determine the stage of the tumor as well as the possibility of nerve or blood vessel involvement and allow him or her to make a treatment plan.
Bone Scan
This test detects bone injury, bone loss and infections by using a harmless amount of radiation. It helps to confirm the diagnosis made by x-ray. Bone scan also helps to determine the metastasis stage of the cancer throughout the skeleton.
PET (Positron Emission Tomography) scan
PET scan also uses radioactive substances for imaging the changes in various cells in the body. The diagnostician injects some radioactive-tagged glucose into the bloodstream to see if any tissue uses more than the normal amount of glucose. These tissues are then scanned for tumors.
Radiographs
Radiographic images can show an “onion skin” appearance of the bones around the tumor due to periosteal reaction.
Biopsy
A small sample can be removed from the suspected tumor and sent for examination (biopsy). The sample is then analyzed under a microscope for detecting any cancer cells present. In some cases, a bone marrow biopsy is required to determine whether the cancer has metastasized to bone marrow.
Bone Marrow Aspiration
In this procedure, a diagnostician collects a small quantity of the bone marrow fluid from the hip bones of a patient. Sometimes, solid tissues from the bone marrow may also be collected. The samples are then sent to be tested for determining the size, maturity and number of blood cells as well as the abnormal cells.
Blood Test
A CBC or complete blood count test shows if there are any abnormalities in the blood. Any abnormality in the CBC result may suggest metastasis of the cancer to the bone marrow of a patient. A blood test named Lactate Dehydrogenase or LDH can determine the enzyme levels in the blood. Elevated serum LDH level is associated with the condition. Ewing’s sarcoma may also increase the red blood cell (RBC) sedimentation rate.
Ewing Sarcoma Differential Diagnosis
A diagnostician should take care to rule out the presence of the following disorders, that give rise to similar symptoms, while diagnosing this type of bone cancer:
- Osteosarcoma
- Non-Hodgkin Lymphoma
- Neuroblastoma
- Rhabdomyosarcoma
- Osteomyelitis
- Nonrhabdomyosarcoma Soft Tissue Sarcomas
- Rickets
Ewing Sarcoma Treatment and Management
The treatment of this disorder may vary from one patient to another depending on the stage of severity and present symptoms. The cure often includes various approaches including chemotherapy, surgery and radiation:
Radiation Therapy
It is a painless process similar to x-rays. This therapy uses a machine that kills the cancerous cells by high-energy X-ray beams. The beams often damages some normal cells as well, but the healthy cells in the area can easily repair the damaged ones. The main object of the treatment is to damage the tumor cells beyond any recovery. Radiation therapy is often combined with chemotherapy and surgery (rarely). At present, it uses external radiation for destroying damaged cells. Scientists are carrying out studies to determine whether this treatment can be more effective if the radiation is implanted within the body of patients.
Chemotherapy
This treatment involves the use of various drugs that kills the cancer cells. The drugs can be administered as oral tablets or injected into a muscle or vein. Chemo is referred to as a systemic treatment as the drugs used in the therapy travels to the affected body parts, with the bloodstream, to destroy all the tumor cells throughout the body. It is called combination chemotherapy when it uses multiple medicines. In the treatment of ESFT, chemotherapy is sometimes used to kill the remaining cancer cells after radiation therapy or surgery.
Surgery
Surgical intervention may be required in some cases for removing the tumor. Sometimes, a surgery is performed for removing remnants of the tumors after chemotherapy. Surgery is performed only if it is impossible to clear the tumor by the other treatment options.
Amputation may be necessary in severe cases where the tumor attaches itself to blood vessels and nerves. In this method, the affected limb is surgically removed along with the tumor.
Myeloablative Therapy
Myeloablative Therapy, along with stem cell support, is mainly used as supplement therapy to the treatments mentioned above. It is used only to treat patients with resistant or recurring Ewing’s Sarcoma or a widely disseminated cancer. All rapidly dividing cells in the body are destroyed by this intense chemotherapy regimen. These include hair cells, blood cells as well as the tumor cells. The self-renewing stem cells create all types of blood cells and other important cells that circulate with blood. This treatment involves stem cell support which helps the stem cells to produce these cells in large amounts after the chemotherapy kills all the cancerous cells.
Treatment may include high-dose chemotherapy and stem cell transplantation, depending on the stage and severity of the cancer.
Ewing Sarcoma Alternative Treatment
Various natural and alternative methods, including the following, are used for its treatment:
- Acupuncture
- Massage therapy
- Herbal products
- Vitamins and other nutritional supplements
- Special diets
Ewing Sarcoma Prognosis
The prognosis is determined by a number of factors including the extent, location and size of the tumor, how it responds to therapy as well as the age and health of patients. His or her tolerance of specific procedures, medications and therapies along with the metastasis stage of the cancer also play important roles in determining the outcome.
Early diagnosis and prompt treatment are very important for having the best possible outcome. Patients should receive regular follow-up care for any signs of recurrence.
Ewing Sarcoma Incidence
Three out of every one million people develop the condition every year in the United States. It is most common in individuals aged between 10 and 20 years with the average age of onset being 15 years. However, it can also occur in adults above 30 years of age. The tumor affects both males and females at the ratio of 1.6:1.
Ewing Sarcoma Survival Rate
The survival rate for patients of this disease has increased considerably over time. At present, the survival rate for children aged below fifteen years ranges between 70% and 75%, while patients who are 15 years to 19 years old have a survival rate of 20% to 49%. Individuals who do not develop metastasis have better chances of surviving compared to those with metastasized tumors.
Ewing Sarcoma Support Groups
There are numerous forums and foundations that provide guidelines about this cancer to spread awareness and to help the patients. These organizations include:
American Cancer Society, Inc.
1599 Clifton Road NE
Atlanta, Georgia 30329
United States
Tel: (404)320-3333, (800)227-2345
Website: http://www.cancer.org
National Coalition for Cancer Survivorship
1010 Wayne Avenue
7th Floor
Silver Spring, Maryland 20910
Tel: (301)650-9127
Fax: (301)565-9670
Email: [email protected]
Website: http:// www.canceradvocacy.org
Sarcoma Foundation of America
9884 Main Street
Damascus, MD 20872
USA
Tel: (301)253-8687
Fax: (301)253-8690
Email: [email protected]
Website: http://www.curesarcoma.org
Ewing’s Sarcoma is a life threatening disorder, associated with a considerable mortality rate. Early diagnosis, along with immediate treatment, is required to extend the life expectancy of sufferers. Patients are allowed to return to their normal lifestyle after treatment. However, regular follow-up is necessary to prevent the tumors from recurring.
References:
http://www.
http://www.mayoclinic.org/
http://www.childrenshospital.
http://www.royalmarsden.nhs.
http://orthoinfo.aaos.org/
The post Ewing’s Sarcoma appeared first on Prime Health Channel.
]]>The post Retinoblastoma appeared first on Prime Health Channel.
]]>It is the name given to a rare type of malignant tumor arising in a part of the eye known as the retina. It generally arises in the early years of childhood, typically before 5 years of age.
The condition is also known by the following names:
- Cancer – retina
- Tumor – retina
Retinoblastoma ICD9 Code
The ICD9 Code for this disorder is 190.5.
Retinoblastoma Incidence
The condition affects 250-350 children in the United States on an annual basis. It accounts for around 4% of all cases of cancer in children who are less than 15 years old, particularly those under 6 years of age. It is most commonly detected in kids aged 1-2 years.
Retinoblastoma Types
The disorder is categorized into a number of types, which include the following:
Unilateral Retinoblastoma
It is the form of the condition that affects only one eye of an individual. In this disorder, tumors are only present in one eye. The majority of patients develop a single tumor in only one eye.
It is the most prevalent type of Retinoblastoma that affects around 60% of all sufferers. Around 85% patients with this form of the disease do not have a hereditary form of the condition.
Bilateral Retinoblastoma
It refers to Retinoblastoma that affects both eyes of an individual. It is observed in around 1/3rd of all sufferers of the condition. The disorder arises in kids born with a mutation in the gene RB1. Hereditary Retinoblastoma may manifest itself as either unilateral or bilateral.
Trilateral Retinoblastoma
It is the form of the condition that affects the pineal gland of sufferers. The pineal gland is a small endocrine gland situated within the brain, under the posterior section of the corpus callosum, which secretes melatonin. Trilateral Retinoblastoma (TRB) is a well-recognized, although rare, condition.
It is also known by various other names, such as Pineoblastoma and Primitive neuroectodermal tumour (PNET). The disorder affects around 5% kids with a constitutional RB1 mutation.
Retinoblastoma Symptoms
The condition may affect one or both eyes of an individual. In children with this disorder, the pupils may develop white spots or even appear white in appearance. In flash photographs, a white glow is often seen in the eyes of sufferers. The pupil may look distorted or white instead of the ‘red eye’ that is typically observed in photographs taken with a flash.
Some other signs and symptoms, that are commonly observed, include:
- Double vision
- Poor vision
- Crossed eyes
- Eyes that do not align
- Redness
- Eye pain
- Varying colors of iris in each eye
Bone pain and other problems may ensue in case cancer spreads to other regions of the body.
Retinoblastoma Causes
The condition results from a mutation in a gene that controls the division of cells. This makes cells grow abnormally and turn cancerous. In around half of all cases of Retinoblastoma, the mutation arises in children without any family history of eye cancer. Naturally, a hereditary cause is ruled out.
In other cases, the mutation is found to be present in several members of the same family that an affected child comes from. There is a 50% risk of the children of a Retinoblastoma sufferer to get the mutation if it is found to run in the family. Therefore, they would have a greater risk of developing the condition themselves.
Retinoblastoma and Genetics
The majority of cases of this disorder arise as a consequence of mutations in RB1, a tumor suppressor gene that usually regulates the growth of cells and prevents rapid or uncontrolled division of cells. Most RB1 gene mutations prevent it from manufacturing any functional protein. Naturally, it is unable to regulate cell division in an effective manner. As a consequence, some retinal cells can divide in an uncontrolled manner to form malignant tumors.
According to some studies, additional changes in genes can influence the occurrence of Retinoblastoma. These changes may help explain differences in the growth and development of tumors in various individuals.
A small number of cases of Retinoblastoma occur as a result of deletions in the chromosome 13 area that contains the RB1 gene.
Retinoblastoma Diagnosis
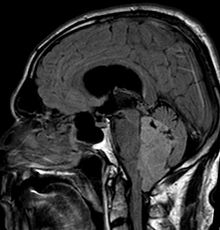
The diagnosis of the disease begins with physician performing a complete physical examination, which includes an eye test. This may be followed up by these exams:
- MRI or CT scan of the head
- Ultrasound exam of the eye (echoencephalogram of the head and eye)
- Eye exam, with pupil dilation
- Examination of Cerebrospinal fluid (In case of aggressive tumors)
- Biopsy of the bone marrow (In case of aggressive tumors)
Sometimes, doctors may recommend the use of anesthetics for a more accurate exam to keep an affected child still during the initial stages of diagnosis.
Imaging tests help doctors find out whether or not the condition has spread to affect other adjoining eye structures.
In some cases, a doctor may recommend patients to other specialist healthcare providers, known as oncologists, who are experts in treating cancerous conditions. Some patients may also be recommended to visit a surgeon or a genetic counselor.
Retinoblastoma Differential Diagnosis
The differential diagnosis for this disorder involves distinguishing its symptoms from those of other similar conditions, such as:
- Coats’ disease
- Incontinentia pigmenti (Bloch-Sulzberger disease)
- Persistent hyperplastic primary vitreous
- Retinal dysplasia
- Retinocytoma
- Retinal astrocytoma
- Retinopathy of prematurity
- Toxocariasis
Retinoblastoma Treatment
The curative options used for treating this disorder depend on the location as well as the size of the tumor. Cryotherapy or laser surgery may be used for curing small tumors. Radiation is implemented for both larger and local tumors.
Chemotherapy
If the tumor is found to spread beyond the eye, Chemotherapy might be required. This is a medicinal treatment that uses chemicals to destroy cancerous cells. The drugs can be administered in a pill form or injected through the blood vessels. The drugs travel all through the body to destroy the malignant cells.
Chemotherapy may also be implemented in curing Retinoblastoma that spreads to tissues in other regions of the body or those external to the eyeball.
In kids suffering from Retinoblastoma, this therapy may help shrink a tumor. Another process, such as Thermotherapy, Cryotherapy, Laser therapy or Radiation therapy may be used to cure the rest of the cancerous cells. This may negate the requirement of surgical cure for affected children.
Enucleation
If the tumor fails to respond to other treatment approaches, a process known as Enucleation may be used to remove the affected eye. In case of some sufferers, especially those in the advanced stages, this may be the first treatment option.
Retinoblastoma Prognosis
The outcome of this disorder is generally positive. Almost every patient can be successfully treated if the cancer does not spread beyond the eye. However, some cases may need aggressive treatment and require even removal of the affected eye to be cured successfully.
If the cancer spreads beyond the eye, the chances of a cure are reduced. Recovery depends on the manner in which the tumor has spread.
Retinoblastoma Complications
The disorder may give rise to a few complications, which can be physically and emotionally extremely disturbing for sufferers. The affected eye may turn blind. The tumor can spread through the optic nerve to the socket of the eye. The malignant growth may also spread to other regions, like the bones, the lungs and the brain.
Kids who have been treated for Retinoblastoma have a risk of recurrence of cancer in and around the cured eye. Due to this reason, a physician is likely to schedule follow-up exams to detect cases of recurrence of this malignant disease. A doctor may redesign a follow-up exam, especially personalized for a child. In the majority of cases, this is likely to involve exams of the eye every few months for the first few years after the course of treatment for Retinoblastoma comes to an end.
Children affected with the inherited form of this disease are also at an elevated risk of developing other forms of cancer in any region of the body in the years following treatment. Due to this reason, kids with an inherited form of Retinoblastoma may undergo regular exams to be screened for other cancerous conditions.
Retinoblastoma Prevention
It is not possible to prevent the condition as its exact causative factors have not been identified as yet. Families can derive some benefit and understand the risk of development of this disorder by seeking genetic counseling. This is particularly necessary in cases where more than one family member is found to have the disorder, or if Retinoblastoma affects both eyes of an individual. When detected in the early stage, when the tumor is small, cure is possible and vision can be preserved in sufferers.
Retinoblastoma and Genetic Testing
Genetic Testing is very important for people with a family history of the condition. The tests can be used to ascertain whether or not:
- A child with Retinoblastoma is susceptible to other associated malignant conditions
- Other children of a couple are at risk of developing this condition as well as other related cancerous disorders, so that eye exams can be started at an early age
- An individual and his or her partner can pass the mutated gene on to other children born to them in future
A genetic counselor can discuss the benefits and risks of genetic testing and decide whether a couple and their children need to be tested for genetic mutation.
Retinoblastoma Pictures
The following images will help you understand how the eyes of children affected with this condition appear to view.
Picture 1 – Retinoblastoma
Picture 2 – Retinoblastoma Image
If you observe any changes in the eye of your child that resemble the symptoms of Retinoblastoma, get in touch with an eye specialist on an immediate basis. Check whether the eyes of your child appear abnormal in recent photographs. Delay in diagnosis and treatment can impact your child’s vision and affect his or her overall health in future. Timely cure can preserve the vision and let your kid have as normal a childhood as possible. It would also ensure a faster recovery. If you have a family history of the disease, ask a pediatrician when regular eye exams should begin for your child to screen him/her for Retinoblastoma.
References:
http://www.mayoclinic.com/health/retinoblastoma/DS00786
http://ghr.nlm.nih.gov/condition/retinoblastoma
http://www.nlm.nih.gov/medlineplus/ency/article/001030.htm
http://www.patient.co.uk/doctor/Retinoblastoma.htm
The post Retinoblastoma appeared first on Prime Health Channel.
]]>The post Ependymoma appeared first on Prime Health Channel.
]]>Ependymomas are rare type of tumors or gliomas that develop from ependymal cells that line the ventricles as well as from central canal of spinal cord. They can develop in the spine and also in the intracranial areas. In children, these gliomas generally develop in the cerebellum. Intracranial ependymomas commonly develop in the fourth ventricle. In some rare cases, they can also occur in pelvic cavity.
Ependymoma Epidemiology
Ependymomas comprise of nearly 5 to 10% of all pediatric brain tumors and they are known to affect both boys and girls equally. The average age of patients during the time of diagnosis is around 5 years. Around 25 to 40% sufferers are below 2 years of age. Pediatric cases mostly occur in the fourth ventricle around the posterior fossa. Ependymoma accounts for almost 25% of all cases of spinal cord tumors. It also constitutes nearly 5% of all adult intracranial gliomas. Nearly 85% of all ependymoma cases are of benign myxopapillary ependymomas. The condition is sometimes associated with syringomyelia and neurofibromatosis type II.
Ependymoma Causes
The exact factors that lead to the development of these tumors are unknown at the present moment. Research is currently being conducted to determine the possible causes of ependymoma tumors.
Ependymoma Grades
Grading of the ependymoma tumors is done by observing their appearance under a microscope. This can help to understand the rate of their progression. The tumors have been graded into 3 types. The Grade 1 tumors are generally slow-developing, whereas the Grade 3 ones grow more rapidly.
Picture 1 – Ependymoma
Grade 1
It includes Myxopapillary ependymoma, Sub-ependymoma and Sub-ependymal giant cell astrocytoma.
Grade 2
It involves low-grade Ependymoma.
Grade 3
It includes Malignant or anaplastic ependymoma and Ependymoblastoma.
Ependymoma Types
There are numerous types of Ependymoma tumors that may develop on various parts of the cranium or the spinal cord. These include:
- Myxopapillary ependymoma (MPE) – These develop mostly in the conus medullaris and the filum terminale of the spinal cord.
- Sub-ependymoma – These generally occur in fourth ventricle but may also develop in the cervical spinal cord and the septum pellucidum
- Classic ependymomas
- Sub-ependymal giant cell astrocytoma
- Anaplastic ependymoma – These usually occur in the posterior fossa.
- Ependymoblastoma – These generally develop within the supratentorial compartment.
- Extraspinal ependymoma or extradural ependymoma
- Tanycytic ependymoma – These affect the spinal cord.
- Intramedullary ependymoma – These occur in the spinal cord.
Ependymoma Morphology
These lumps are characterized by the growth of cells having regular round to oval-shaped nuclei. A fibrillary background with variable density can be seen. The tumor cells may develop gland-like elongated or round structures that look like embryologic ependymal canal having long, delicate processes that extend into the lumen. The perivascular pseudorosettes that occur frequently have the tumor cells arranged around the vessels having an intervening zone that consists of thin ependymal processes that are directed toward the walls of the vessel. The ependymomas might have originated from the radial glia.
They are found to develop in various parts of the intracranial region, as well as the spinal cord, such as:
- Posterior fossa
- Supratentorium
- Fourth ventricle
- Septum pellucidum
- Cervical spinal cord
Ependymoma Symptoms
Ependymomas are generally slow-growing tumors and their characteristic signs and symptoms may take several months to become apparent. The symptoms tend to depend on the area of the cranium or the spinal cord that is affected. The various signs and symptoms that are commonly associated with these brain tumors include:
- Sciatica
- Nausea
- Seizures
- Scoliosis
- Paralysis
- Vomiting
- Dysphagia
- Drowsiness
- Hemiparesis
- Loss of appetite
- Lower back pain
- Severe headache
- Speech problems
- Memory problems
- Difficulty in sleeping
- Bilateral Babinski sign
- Temporary visual loss
- Weakness of the limbs
- Uncontrollable twitching
- Temporary loss of memory
- Stiffness or pain in the neck
- Inadequate bladder control
- Raised intracranial pressure
- Problems with coordination
- Development of hydrocephalus
- Nystagmus or jerky eye movements
- Obstruction in the flow of the cerebrospinal fluid
- Temporary inability to identify or distinguish various colors
- Seeing horizontal or vertical lines under the presence of bright light
Ependymoma Diagnosis
While diagnosing these tumors, a doctor is likely to first conduct a thorough physical examination to check the reflexes as well as the strength arms and legs of a patient. He or she will then check for any eye symptoms that are commonly associated with this condition. Following a detailed ophthalmic examination, the doctor would also conduct the following medical tests to check the growth of tumors:
- Biopsies
- CT scans
- MRI scans
- Lumbar puncture tests
Ependymoma Differential Diagnosis
There are certain other health conditions which show signs and symptoms similar to that of Ependymoma tumors. Hence, while conducting the diagnosis, a doctor or a diagnostician needs to differentiate it from these similar-appearing conditions in order to choose the best possible mode of treatment. The differential diagnoses for Ependymoma includes ensuring the absence of conditions such as:
- Astrocytomas
- Glioblastoma Multiforme
- Choroid Plexus Papilloma
- Arteriovenous Malformations
- Tumorous growths of the conus medullaris and the cauda equina
Ependymoma Treatment
A number of treatment methods are used to manage these tumors. While deciding on the optimal method of treatment, a doctor keeps in mind the following considerations:
Picture 2 – Ependymoma Image
- Type, size and location of the tumor
- The extent of the disease’s progression
- The patient’s medical history, age as well as overall health
- Expected nature of progression
- Tolerance level for certain procedures, medications or therapies
- Preference and judgment of the patient’s immediate family
Surgery
Surgery is the most common form of treatment for this disorder, and is generally performed first to get rid of tumor as much as possible. The procedure is supervised by a neurosurgeon. Although complete removal of the tumor is the prime goal of the surgery, the tumor’s location or other features may sometimes make it difficult for the medical team to remove it completely.
VP shunt or Endoscopic Third Ventriculostomy (ETV)
If a tumor leads to the blockage of the cerebrospinal fluid (CSF) flow, a team of surgeons might opt for either of the two procedures to relieve signs of hydrocephalus, or build-up of fluid within the skull. A tube known as Ventriculo-peritoneal shunt (VP shunt) might be used to drain excess cerebrospinal fluid into the patient’s abdomen. Alternatively, the same might be achieved by endoscopic third ventriculostomy. In this process, the neurosurgeons create a tiny hole or an incision that allows the fluid to move past the blockage and flow into the patient’s spinal column. Almost 90% cases of pediatric ependymoma are treated in this method.
Radiation Therapy
Precise doses of radiation therapy are targeted to kill the cancer cells that are left behind even after surgical treatment. Radiation therapy is used to check the local metastasis of the tumor. Spreading of an Ependymoma might make it necessary for a doctor to recommend radiation for the whole brain and the spinal cord.
Chemotherapy
Chemotherapy effectively reduces the potential of cancer cells to spread or reproduce. Chemotherapeutic procedures prior to surgery might help to minimize the size of the tumor thereby facilitating its surgical removal. Chemotherapy drugs may be administered orally, intramuscularly, intravenously or intrathecally.
Medications
Medications might be recommended for controlling of seizures.
Ependymoma Prognosis
The outcome of the condition depends on the extent of the tumor resection as well as the age of patients. In some cases, however, the location of the tumor as well as its microscopic characteristics might also influence the overall outcome of the condition. Prognosis is good with total resection of the tumor. Instances of recurrences have been recorded in cases where total resection was not possible. A residual tumor is also most likely to spread through cerebrospinal fluid, which might lead to tumor-related complications. Patients younger than 4 years of age generally have a poorer outcome due to increased incidence of lateral posterior fossa tumor growth.
Ependymoma Survival Rate
The 5-year rate of survival for adult ependymoma patients is around 50% to 55%. Survival rate for children with posterior fossa tumors is significantly less.
Ependymomas are ependyma-related tumors that develop in the spinal cord or cranium. They can cause pressure within the cranium which can cause several complicated symptoms. Treatment needs to be followed up by regular medical checkups for several years to check for any signs of tumor recurrence.
References:
http://www.childrenshospital.org/az/Site841/mainpageS841P0.html
http://www.childhoodbraintumor.org/brain-tumor-types-and-imaging/98-ependymomas.html
http://www.braintumor.org/patients-family-friends/about-brain-tumors/tumor-types/Ependymoma.html
The post Ependymoma appeared first on Prime Health Channel.
]]>The post Liposarcoma appeared first on Prime Health Channel.
]]>Liposarcoma Definition
It is a cancerous soft tissue tumor developing in the fat tissue. It is found to develop most frequently in the extremities or in the abdominal cavity. Although it is usually found to affect the upper arm or the thigh, it can arise on almost any region of the body.
Liposarcoma Incidence
The condition is mostly observed in middle-aged or elderly individuals, usually 40 years or older in age. These are the second-most common types of sarcomas of the soft-tissue (after Malignant Fibrous Histiocytoma). However, only around 1,250 individuals in the U.S are affected by it every year. As is the case of all types of sarcoma, this is an extremely rare growth. Only 2.5 cases of this type of tumor are seen in every 1 million individuals.
The condition affects men slightly more than women. It affects children only rarely. Only about 5% cases of this tumor are reported in kids. In spite of being one of the most common type of sarcomas, Liposarcomas are rare in number.
Liposarcoma Types
Histologically, this tumor is classified into several types:
Well-differentiated Liposarcoma
It is also referred to as Atypical lipomatous tumor, although this term is used to indicate lesions that arising in areas other than the retroperitoneum. These are tumors having low-grade malignancy. These may not metastasize but recur only locally.
These growths have been further classified into three subtypes:
- Inflammatory
- Lipoma-like
- Sclerosing
Dedifferentiated Liposarcoma
It comprises of well-differentiated Liposarcoma that lies next to a tumor that is more poorly differentiated.
Myxoid Liposarcoma
It is also referred to as Round cell Liposarcoma, although the name actually indicates a variant of myxoid growths that are poorly differentiated. It is the rarest type of cancerous tumor to develop in fatty tissue. Most of these tumors develop in the upper arms or the thighs, although there is also the possibility of these growths to arise in other areas of the body as well. These tumors often arise as palpable growths immediately beneath the skin surface that have a slow growth over a period of time. When diagnosed in the initial stages, the myxoid growths can be effectively removed by surgeries and the risk of cancer can be avoided.
These are the most common form of Liposarcoma tumors. They make up for around half of all cases of this type of tumor and have a relatively favorable prognosis.
Pleomorphic Liposarcoma
These are extremely malignant types of tumor and account for 5% of all cases of Liposarcoma. They show an irregular pattern of growth and have an extensive cellular pleomorphism. The median age of development of this growth is 54-70 years. These arise only rarely in childhood.
Mixed Liposarcoma
It refers to a mixture of all the above types of Mixed Liposarcoma. It is rare in occurrence and affects older patients, usually in the retroperitoneum. They are usually large in shape and solid in size. They appear white, yellow or gray in color.
Liposarcoma Symptoms
The condition usually manifests itself as a deep-seated growth in the soft tissue of affected individuals. Such tumors are usually asymptomatic (i.e, not giving rise to any symptoms) in the initial stages. The majority of them are, on an average, anywhere from 0.75 to 4 inch (approx) in size.
However, it results in problems as it gets larger in size. Patients suffer from pain as well as functional disturbances. Large tumors of this type, particularly those developing in the organs, may result in pain or impairment of functions of the organs. Exceptionally large tumors of this type have been reported, although such cases are very rare.
In case of Retroperitoneal tumors, patients may suffer from symptoms such as:
- Abdominal pain
- Weight loss
- Emaciation
The tumors may also compress the ureter or the kidney and cause kidney failure.
As sarcomas of the soft tissue affect tissues that are elastic and can move easily, such type of a tumor may persist for a long duration before it is diagnosed and grows big enough to push adjoining tissue aside. The signs and symptoms arising due to this growth vary to a great extent, depending on factors such as:
- Location of the tumor
- Size of the tumor
- Metastasis of the tumor
However, patients usually experience problems like:
- Soreness or pain resulting from compression of muscles or nerves
- Painless inflammation or growth at any site on the body
- Limping or other difficulties in using body parts like the arms, hands, legs or feet
- Reduced range if motion in the impacted body part
Liposarcoma Causes
Researchers are still at a loss regarding the exact cause of this type of tumor, which is thought to develop from mesenchymal cells. However, they have hinted at some possible factors. These include:
Heredity
Certain studies have indicated a possible link between heredity and the development of sarcomas of the soft tissue. Medical researchers have conducted a study on a few families having several members of one generation suffering from soft tissue sarcomas.
Infection
An association has been indicated between Epstein-Barr viral infection and this tumor.
Disorders
Certain inherited conditions have also been associated to an increase in the risk of origination of soft tissue sarcomas like Neurofibromatosis or Li-Fraumeni Syndrome.
Cancers
A few studies have hinted at a possible relation between some types of cancer and soft tissue sarcomas.
Liposarcoma in Dogs
The condition typically affects older dogs and is referred to as Canine Liposarcoma. The condition has a poor prognosis in canines; dogs are found to die more frequently than humans affected by this type of tumor. It is believed to be result of harmful alterations in the DNA of dogs, as they grow older in age. However, pets have a greater chance of having a recovery if this type of growth is surgically removed in the initial stages of its development. However, such lumps are found to recur in certain cases.
In dogs, the condition manifests in the form of tangible growths as well as symptoms like:
- Difficulties in eating
- Lack of appetite
- Changes in movement or gait
- Persistent pain in the joints
- Swollen legs
- Abdominal lumps
Liposarcoma Diagnosis
This tumor is diagnosed through a histological examination of the soft tissue, such as an excisional biopsy. Patients are often detected with Lipoblasts, cells containing lots of clear multi-vacuolated cytoplasm and a dark-staining nucleus.
The tests that are typically used to detect this form of tumor include:
- MRI scans
- CT scans
Liposarcoma Differential Diagnosis
The differential diagnosis of these tumors includes taking into account other conditions that give rise to similar symptoms. Physicians should make sure that patients are experiencing problems caused by Liposarcoma and not other conditions like:
- Other types of Sarcomas, like Leiomyosarcoma and Fibrosarcoma
- Malignant Fibrous Histiocytoma (MFH)
- Lipoma
- Neurofibromatosis
- Fatty retroperitoneal lumps, such as Myelolipoma ad Angiomyolipoma
Liposarcoma Treatment
The treatment for this disease can be invasive or non-invasive.
Invasive treatment
It involves use of surgical methods to remove the cancerous growth. This can include any of the following techniques:
Wide-local excision
It involves removal of cancerous tissue, along with some of the adjoining healthy tissue.
Limb-sparing surgery
In this process, multiple surgical methods are used to remove the tumor without amputating the limb.
Amputation
Surgeons remove an entire limb or a part of it to remove large tumors or those formed in complex areas.
Non-invasive treatment
These include any of the following measures:
Radiation therapy
It may be used before or after operation to lower the risk of recurrence.
Chemotherapy
It is used to shrink the tumor prior to surgery or destroy small cancerous cells in other regions of the body that are undetectable even with advanced imaging exams.
Liposarcoma Prognosis
The outcome of the condition tends to vary based on the location where the tumor originates as well as other factors like:
- Size of the tumor
- Depth of the tumor
- Type of malignant cell
- Nearness to the lymph nodes
With radiation therapy and surgery, well-differentiated types of this tumor tend to recur only in about 10% cases. Metastasis of these growths is also uncommon. The 5 year survival rate associated with this type tends to vary between 39 and 100%, depending on histological subtype.
Almost all individuals affected by the Well-differentiated types are found to survive even 5 years after the removal of the tumor. The Myxoid types are related with an 88% rate of survival. However, death rate is relatively higher in case of Liposarcomas that are poorly differentiated.
Lipoma Vs Liposarcoma
Lipoma refers to an adipose tumor or a type of tumor comprising of fatty tissue. These are almost always benign (non-cancerous) and are most frequently found to arise in the subcutaneous tissues although they may also be observed in other deeper tissue regions like the abdominal organs or the intermuscular septa. Liposarcoma, on the other hand, is a sarcoma or malignant tumor containing fat cells. These appear in a fashion similar to Lipoma and are usually more common on the shoulders, lower extremities and in the retroperitoneum.
Liposarcoma – Information and Support Organizations
Patients of Liposarcoma, and their family members, can get in touch with any of the following organizations for necessary information, support and advice related to this type of sarcoma.
Genetic Alliance
4301 Connecticut Avenue NW
Suite 404
Washington, DC 20008-2369
Telephone: 202-966-5557
Fax: 202-966-8553
E-mail: [email protected]
Web site: http://www.geneticalliance.org
National Organization for Rare Disorders (NORD)
55 Kenosia Avenue
PO Box 1968
Danbury, CT 06813-1968
Toll-free: 1-800-999-6673 (voicemail only)
Telephone: 203-744-0100
TTY: 203-797-9590
Fax: 203-798-2291
E-mail: [email protected]
The Liddy Shriver Sarcoma Initiative
17 Bethea Drive
Ossining, New York 10562-1620
Telephone: 914-762-3251
Fax: 914-941-9181
E-mail: http://sarcomahelp.org/about.html?tpm=1_3
Web site: http://sarcomahelp.org/
Liposarcoma Pictures
The following images will help you get an idea about the appearance of these tumors.
Picture 1 – Liposarcoma
Picture 2 – Liposarcoma Image
If you have been experiencing painful symptoms in the limbs or abdomen or suffering from weight loss for some time now, it is imperative for you to get in touch with a physician and get yourself diagnosed properly. Lack of proper and timely diagnosis and treatment can complicate your condition and earlier medical attention is always necessary in case of malignant conditions such as Liposarcoma.
References:
http://en.wikipedia.org/wiki/Liposarcoma
http://rarediseases.info.nih.gov/GARD/Condition/6913/Liposarcoma.aspx
http://www.childrenshospital.org/az/Site1096/mainpageS1096P1.html
http://www.vetinfo.com/liposarcoma-symptoms-in-dogs.html#b
The post Liposarcoma appeared first on Prime Health Channel.
]]>