What is Non Alcoholic Fatty Liver Disease
Page Contents
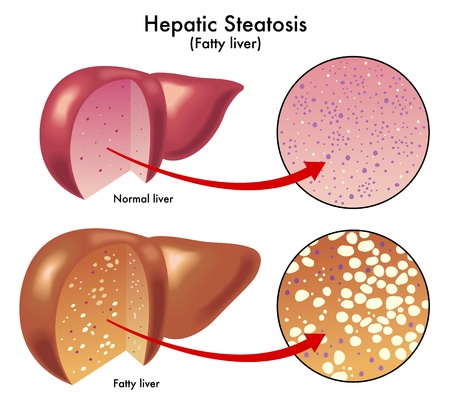
Non-alcoholic fatty liver disease or NAFLD constitutes a group of conditions in which excess fat accumulates in the liver of people who drink little or no alcohol.
Nonalcoholic Steatohepatitis
Nonalcoholic steatohepatitis (NASH), a more serious form of the disease, occurs when, along with the fat build up, there is inflammation and subsequent irreversible damage to the liver.
Signs and Symptoms
Both NAFLD and NASH may have no symptoms at the early stage. However, if they do occur, one may encounter:
- Abnormal or sudden weight loss
- Weakness and fatigue all the time
- Persistent upper abdominal pain
Causes
It is not clear why NAFLD occurs in some people. However, some studies holding environmental factors to be the cause, point out that overconsumption of certain nutrients like cholesterol, iron or refined sugar, may result in an excess amount of fat that neither breaks down nor gets eliminated, thereby leading to the condition.
According to some other studies, genetic changes may also be responsible for the condition. Instructions given by the PNPLA3 gene results in formation of a protein believed to regulate the development and breaking down of fats. The activity of this gene decreases when one fasts, increasing immediately again with food intake – the production of the protein varying as per the requirements of the body. When someone has irregular eating habits, the normal working of the gene disrupts; it can no longer break down fat smoothly and thus surplus fat is formed. Also, a variation of the gene may lead to a decrease in the breakdown of fat by the protein, thus resulting in excess fat.
Though it is also not known why NAFLD degenerates into NASH, certain studies have put forward some mechanisms as responsible for the inflammation of NASH. These are:
- Release of toxic inflammatory chemicals by fat cells
- Self-destruction or apoptosis of liver cells
- Effects of free radicals (oxidative stress)
- Effects of intestinal microorganisms on nutrient breakdown and absorption
- Abnormal reaction of the immune system to surplus fatty tissues in the liver
Risk Factors
The common risk factors of both NAFLD and NASH include:
- Obesity, particularly the concentration of fat in the belly
- Resistance to insulin
- Elevated blood sugar levels suggesting type 2 Diabetes
- High levels of fat, chiefly triglycerides, in the blood
- Metabolic syndrome
Other than these, possible associated conditions behind the development of only NAFLD include:
- Polycystic ovary syndrome
- Sleep apnea
- Underactive thyroid (hypothyroidism)
- Underactive pituitary gland (hypopituitarism)
- In rare cases, medicines such as methotrexate and tamoxifen
- Fast loss in weight induced due to surgery
- High blood pressure (hypertension)
Complications
- Type 2 Diabetes
- Cardiovascular diseases
- Cirrhosis or late-stage scarring (fibrosis) of the liver
- Gallstone disease (GD)
Diagnosis and Tests
NAFLD, being asymptomatic, mostly remains undetected. It is only when certain tests done for other reasons refer to a liver problem, when the condition is suspected. Tests undertaken to confirm the condition and rule out other diseases include:
- CBC (Complete blood count)
- Chronic viral hepatitis (hepatitis A, hepatitis C, and others) tests
- Liver enzyme and liver function tests to look for an unusual liver or abnormal levels of the liver enzymes, alanine aminotransferase (ALT) and aspartate aminotransferase (AST)
- Screening test for celiac disease
- Blood sugar fasting
- Hemoglobin A1C, to determine the stability of blood sugar
- Lipid profile, to measure blood fats, such as cholesterol and triglycerides
Imaging Tests
Plain ultrasound, computerized tomography (CT) scanning, and magnetic resonance imaging (MRI) are often the initial tests done for detecting any liver abnormality. While transient elastography, and magnetic resonance elastography are done to measure liver stiffness, which may suggest fibrosis or scarring
Liver Biopsy
If the above tests do not confirm the condition, a small tissue from the liver is taken to check for signs of inflammation or scarring (biopsy).
Treatment and Management
Self-Regulation
At present, no medical treatments are available for NAFLD and NASH. However, certain lifestyle changes that can help manage the conditions are:
- Weight loss through regular exercise
- Abstaining from drinking alcohol and smoking
- Controlling diabetes and cholesterol
- Protecting the liver
Diet Tips and Restrictions
Since excess fat can generate the condition, care should be taken to maintain a healthy diet.
Foods to Eat
- Choline-rich (a B complex vitamin) foods such as cauliflower, mushroom, and eggs
- Monosaturated fatty acids, present in vegetable oils like sesame, olive, canola, and peanut
- Fiber-rich foods like lentils, black beans, broccoli, and Brussels sprouts
Recent studies suggest drinking coffee may be associated with a lower risk of the NAFLD symptoms deteriorating and advancing to NASH.
Foods to Avoid
- Eatables made from palm or coconut oil
- Baked goods
- Meat and dairy products
Current Concepts and Management Strategies
- According to recent studies, weight reduction through bariatric surgery may help severely obese people with NAFLD. Administration of the drug metformin may also help with improving the insulin resistance of NAFLD affected people.
- In case of NASH, the two experimental approaches that are gaining prominence include the administration of supplements such as vitamin E and vitamin D, selenium, and betaine, and a liver transplantation. However, more research needs to be done in these areas.
In Pregnancy
There is scarce data available regarding the association of NAFLD with pregnancy. As per certain individual case studies, the condition does not pose any threat to either the mother or her baby as long as it does not develops into NASH.
Prognosis and Life Expectancy
NAFLD is usually curable and most people recover after following a restricted lifestyle, and treatment regime, going on to have normal life expectancy. However, the condition may return in some cases or lead to NASH, liver cirrhosis and even cause death. It is estimated that among 100 people suffering from NAFLD, about 2 develop cirrhosis over 15-20 years; whereas, nearly 12 among 100 people with NASH have cirrhosis over about 8 years.
Incidence and Prevalence
About 20‑30% of US population is affected by NAFLD, whereas about 2‑3% has NASH.
NAFLD and NASH ICD-9-CM Codes and ICD-10-CM Codes
The ICD-9-CM code of NAFLD is 571.8, and ICD-10-CM code is K76.0
The ICD-9-CM code of NASH is 571.8, and ICD-10-CM code is K75.81