Have you been suffering from loss of visual capabilities from time to time these days? The problem could be an ocular condition known as Optic neuritis (ON). Read and know all about this disease, including its possible symptoms, causes, diagnosis and treatment options.
Optic neuritis Definition
Page Contents
- 1 Optic neuritis Definition
- 2 Optic neuritis ICD9 Code
- 3 Optic neuritis Incidence
- 4 Optic neuritis Symptoms
- 5 Optic neuritis Causes
- 6 Optic neuritis Diagnosis
- 7 Optic neuritis Differential Diagnosis
- 8 Optic neuritis Treatment
- 9 Optic neuritis Management
- 10 Optic neuritis Risk Factors
- 11 Optic neuritis Complications
- 12 Optic neuritis Prognosis
- 13 Optic neuritis Recovery Time
- 14 Optic neuritis Pictures
It refers to a swelling of the optic nerves, the cluster of nerve fibers that supply visual information from the eyes to the brain. Inflammation of these nerves results in pain and abruptly reduced vision in the affected eye. The loss of vision is usually temporary in nature.
The condition is also known by the name “Retro-bulbar neuritis.”
Optic neuritis ICD9 Code
The ICD9 Code for this condition is 377.30.
Optic neuritis Incidence
The disease usually affects adults in the age group of 18-45 years. The mean age of occurrence of the condition is 30-35 years. ON is more common in females. Annually, the disease affects 5 out of 100,000 individuals.
Optic neuritis Symptoms
The problem is primarily characterized by one or more of the following symptoms:
Loss of color vision
Patients often complain about their perception of colors being affected. Affected individuals may notice prominent colors, such as red, being less vivid than usual or apparently faded.
Loss of vision
Vision loss usually affects one eye for an hour or a period of few hours. The majority of sufferers have temporary loss of vision of this type. In case of a prominent vision loss, the condition generally persists for several hours or even days. The problem may be aggravated with exercise or heat. In some cases, the absence of visual capability may be permanent.
Pain on moving the affected eye
The majority of sufferers report of pain that is worsened as they try to move their eyes to view people or objects. The painful symptoms related with the condition usually peak in the course of a few days.
Altered bright light response
Some individuals suffer from changes in the manner of response of the pupil to bright light. In some cases, affected individuals may also report of seeing flickering or flashing lights.
In some cases, such signs and symptoms may indicate the presence of an autoimmune disorder known as Multiple sclerosis. Optic neuritis is usually the first problem that is reported in around 15-20% individuals who develop this autoimmune disease.
Optic neuritis Causes
It is not known what exactly leads to this disorder. The condition is supposed to arise when the immune system wrongly targets the myelin sheath over the optic nerve, leading to the swelling and damage of the sheath.
In healthy individuals unaffected by the condition, the myelin helps in quick transmission of electrical impulses along the optic nerve, to the brain from the eye. The electrical impulses are converted to visual information in the brain. In people affected by ON, this transmission of visual information is affected. It is not known what exactly leads to a swelling and damage of the myelin sheath and gives rise to ON.
However, researchers have associated ON to certain conditions. These include:
- Multiple sclerosis
- Cranial arteritis
- A fungal infection known as Cryptococcosis
- Autoimmune disorders, including Behcet’s disease, sarcoidosis, neuromyelitis optica and lupus
- Bacterial infections, which include syphilis, meningitis, tuberculosis and Lyme disease
- Respiratory infections, which include common upper respiratory tract infections and Mycoplasma pneumonia
- Viral infections, that include measles, chickenpox, rubella, viral encephalitis,mononucleosis, mumps and herpes zoster infections
Some other factors, that have been linked to the occurrence of ON, include:
- Drugs, such as Ethambutol
- Radiation therapy
- Any condition that can lead to the compression or inflammation of the optic nerve, such as toxins, tumors or malnutrition
Optic neuritis Diagnosis
The diagnosis of the condition usually involves:
Physical examination of the eye
Eye doctors usually check the vision of sufferers and assess their ability to perceive various colors.
Ophthalmoscopy
In this process, doctors shine a bright light over the eye of patients and check the structures present at the back of the eye. The test makes an evaluation of the optic disc, the point of entry of the optic nerve into the eye. In around one third of all ON sufferers, the optic disc gets inflamed.
Pupillary light reaction test
The technique involves moving a flashlight before the eyes to check the response of the pupils on exposure to bright light. Pupils affected by ON do not constrict as much as eyes normally do when stimulated by light.
In some cases, doctors may order for some additional tests like:
Blood tests
These are used to detect the presence of antibodies for neuromyelitis optica. Those with acute ON may go through this exam to assess whether they are susceptible to neuromyelitis optica. An ESR blood test is used to check for swelling in the body. The exam may help in assessing whether cranial arteritis (inflammation of cranial nerves) is responsible for ON.
Visual response test
The exam is able to detect the retardation of electrical conduction from optic nerve areas that have become damaged.
Brain MRI scan
MRI of the brain is conducted with the aid of special optic nerve images. During an MRI conducted for detecting ON, patients are injected with a contrast solution. The solution makes the optic nerve and various other brain areas more visible on the images. MRI is also important in determining whether certain regions of the brain have suffered any damage. The presence of lesions in the brain indicates a high risk of development of Multiple Sclerosis.
Certain medical exams may help rule out the presence of associated conditions. These include:
- Visual field testing
- Visual acuity testing
- Color vision testing
- Optic disc examination by Indirect Ophthalmoscopy
Optic neuritis Differential Diagnosis
The differential diagnosis of Optic neuritis involves distinguishing its signs from those of other conditions that give rise to similar symptoms. These include:
- Acute Glaucoma
- Anterior Ischemic Optic Neuropathy
- Compressive Optic Neuropathy
- Interstitial Keratitis
- Meningioma of Optic Nerve Sheath
- Sarcoidosis
- Sudden Visual Loss
- Thyroid Ophthalmopathy
- Toxic or Nutritional Optic Neuropathy
Diagnosticians should make sure that the problems experienced by patients are not the result of the abovementioned disorders.
Some other conditions that physicians should consider during differential diagnosis, include:
- Branch retinal artery occlusion
- Central retinal artery occlusion
- Hereditary optic neuropathies
- Herpes simplex
- Neuromyelitis optica
- Nutritional optic neuropathies
- Wegener granulomatosis
- Necrotizing herpetic retinopathy in immunocompromised individuals
Optic neuritis Treatment
ON usually resolves on its own but in some individuals, physicians may use steroid medicines to reduce optic nerve inflammation and treat ON. However, steroid treatment may give rise to certain possible side effects such as:
- Insomnia
- Weight gain
- Stomach upset
- Changes in mood
In cases where steroid therapy fails to cure the condition and acute loss of vision continues, a treatment option known as Plasma exchange therapy may be used to help some patients recover their visual ability.
Medications may prove to be useful in curing acute cases of the disease. Intravenous (administered through vein) administration of corticosteroids may be useful in speeding up the pace of recovery. Physicians should use higher doses with caution as acute side effects have been known to be associated with the use of too much corticosteroids.
While use of methylprednisolone quickens the pace of recovery in the severe stages of ON, they are found to have no effect on the final visual acuity of sufferers. Oral prednisolone is not generally recommended as certain unconfirmed studies suggest that they may elevate the risk of recurrence in affected individuals.
Optic neuritis Management
In patients suffering from a worsening of ON symptoms due to raised body temperature, doctors recommend avoiding hot surroundings and consuming cool drinks to maintain lower body temperature. Physicians should assure sufferers that the symptoms are reversible and do not usually cause greater damage to the vision.
Optic neuritis Risk Factors
The risk factors for ON, arising from autoimmune conditions, include:
Age
Although ON may develop at any age, it is most often evident in young adults aged between 20-40 years. The average age of onset of the condition is around 30 years.
Sex
The disorder affects women two times more than men.
Race
The condition is more common in white population than black ones.
Genetic mutations
Certain mutations in gene may elevate the risk of development of ON or multiple sclerosis.
Optic neuritis Complications
The condition may give rise to a number of complications, which include:
Reduced visual acuity
The majority of sufferers regain their vision partially or almost completely within a period of several months. In some people, however, the loss of vision may continue even after ON has resolved.
Damage to the optic nerve
Most affected individuals, following an episode of ON, suffer from some permanent damage of the optic nerve. However, they may not experience any symptoms occurring due to this damage.
Side effects of cure
As aforesaid, patients may suffer from side-effects due to steroid treatment. Steroid medicines used to cure ON subdue the immune system. This makes the body more vulnerable to infections. Prolonged use of steroids may also result in thinning of the bones, a condition known as Osteoporosis.
Optic neuritis Prognosis
The outcome of the disorder is usually good. The majority of sufferers of ON regain their vision almost completely within a year after the onset of the condition. In some cases of Acute ON, patients may have a recurrence of the condition in either eye. Most people suffering from a single episode of the disease eventually gain their vision back. Treatment with steroid drugs may quicken recovery of vision after the development of this disease.
In patients of ON found to be at an elevated risk of having Multiple Sclerosis (MS), based on MRI findings, doctors are likely to use medications to prevent the development of MS.
Optic neuritis Recovery Time
The visual abilities of ON sufferers usually return within 2 to 3 weeks even without any treatment measures.
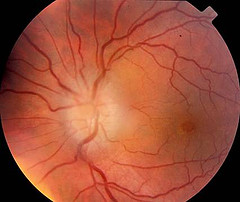
Optic neuritis Pictures
The following images show the physical appearance of ON patients.
Picture 1 – Optic neuritis
Picture 2 – Optic neuritis Image
If you, or any of your family members, are suffering from short-term loss of vision, it is important to seek immediate diagnosis and treatment for the condition. Timely diagnosis and cure can be helpful in restoring visual capability and avoiding progression of ON and occurrence of complications in future.
References:
http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001750/
http://www.mayoclinic.com/health/optic-neuritis/DS00882
http://www.patient.co.uk/doctor/Acute-Optic-Neuritis.htm
http://en.wikipedia.org/wiki/Optic_neuritis