The post Hyperhidrosis | Causes, Symptoms, Diagnosis & Treatments appeared first on Prime Health Channel.
]]>Hyperhidrosis is unusual and extreme sweating which is not associated with exercise or heat. A person sweats so much that it drenches through clothes and seeps through hands. Besides disturbing regular activities, excessive sweating can result in embarrassment and social anxiety. It is a common disorder and over 5% -10% of Americans suffers from it.
What body parts are usually affected?
Hyperhidrosis in sole and palm sweating begins around the age of 13 while underarm sweating starts after maturity. If the problem is left untreated, it can continue throughout the life. In severe cases, serious issues are seen like problem in holding a pen, shaking hands or gripping a steering wheel. It can also make it hard to lead a healthy life. It can affect a specific body part or the entire body. However, feet, palm, underarm and groin are the most common parts affected due to the maximum number of sweat glands.
Types
- General Hyperhidrosis: Not limited to any specific body part, it occurs throughout. It is often called secondary
- Palmer Hyperhidrosis: The medical term used for impacting palms, it is the most common form that affects social interactions and healthy
- Plantar Hyperhidrosis: Impacts feet or soles, easy to hide with socks and shoes. It also makes it difficult condition by making feet slippery.
- Axillary Hyperhidrosis: Affects underarm area, it has the highest density of sweat glands, and people usually sweat heavily in this section after an extreme But patients with this disorder sweat naturally without any exercise and the sweat leaves a stain on the garment which results in self-consciousness and nervousness.
- Facial Hyperhidrosis: Excessive sweat on face and head, it is the most embarrassing as it harms a person’s social life.
- Truncal Hyperhidrosis: Impacts the groin area, thigh region, and These regions are prone to fungal infections as they take a longer time to dry.
Types Based On Repressed Health Condition
- Primary Idiopathic Hyperhidrosis: Condition when the reason of abnormal sweating is unknown. In most of the cases, hyperhidrosis is limited.
- Secondary Hyperhidrosis: Person sweats due to hidden health condition like gout, obesity, tumor, menopause, diabetes mellitus, mercury poisoning, hyperthyroidism, etc.
Causes
Primary Causes
- Anxiety
- Emotional Stress
- Panic attacks
- Nervousness
- Certain genes
Secondary Causes
- Alcohol abuse
- Spinal cord injury
- Anxiety
- Gout
- Diabetes
- Heart Disease
- Obesity
- Hyperthyroidism
- Pregnancy
- Parkinson ’s disease
- Shingles
- Respiratory Failure
- Infections (Tuberculosis, Malaria & HIV)
- Substance abuse
- Cancer
- Medications including, antidepressants, pilocarpine (for glaucoma), anticholinesterases (for Alzheimer’s disease), propranolol (for hypertension)
Symptoms
Physical Symptom
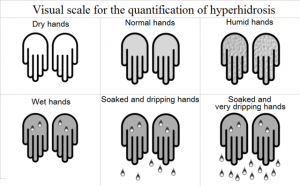
- Wet hands or moist hands
- Wet soles or damp feet
- Frequent sweating
- Excessive sweating that drenches outfit
- Irritating & Painful skin problems (bacterial or fungal infections)
Physiological Symptom
- Self-conscious
- Hesitation to make physical contact
- Withdrawn socially, sometimes leads to depression
- Disturbed about stained clothing
- Worrying about body odor
- Spending a substantial time managing sweat, like wiping, using napkins and pads below arms, wearing dark or heavy clothes, changing clothes, etc.
Risk Factors
- Genetics: Genetic tendency can lead to primary hyperhidrosis.
- Menopause: Women experience a different type of physical and emotional change which can lead to extreme sweating.
- Puberty: Adolescents steadily are exposed to stress and anxiety leading to severe sweating.
- Nerves and Brain Functions: Impaired neural brain response can provoke the sweat glands to react to body temperature wrongly.
- Obesity: Hyperhidrosis affects any body type, but overweight people are more prone to the disease as the sweat glands work twice to clean the toxins and also maintain the body temperature.
- Temperature: Sweat controls the body temperature when exposed to intense humidity and heat. The body requires cooling by excessive sweating to manage temperatures. Hence, people living in colder climate sweat more when they are exposed to high temperatures.
Other disorders include different type of cancers, Hodgkin’s disease, frequent infections like HIV, tuberculosis and Parkinson’s disease.
Diagnosis
The doctor will examine for some underlying conditions first, like low blood sugar levels, or overactive thyroid through blood tests. Patients will be asked about the sweat pattern like body part affected, sweating episodes, whether they sweat during sleep, etc. Additionally, an expert might also ask a series of questions or ask to fill out a questionnaire to know the details.
- Thermoregulatory sweat test: Powder that is moisture sensitive is applied to the skin which changes its color due to excessive sweating. Patients are exposed to high temperature, and people with hyperhidrosis will excessively sweat on palms. It allows the doctors to know about the seriousness of the condition.
Treatment
It usually starts with the antiperspirants. Other therapies and medications are available if antiperspirants don’t work. In some severe cases, experts might suggest a surgery to separate the nerves liable for sweat overproduction or to remove sweat glands.
- Iontophoresis: Hands and feet are submersed in water to pass a comfortable electric current. Most patients require three to five 25-35 minute treatments.
- Anticholinergic drugs: Medicines stops the delivery of parasympathetic nerve impulsions. It takes about two weeks to show valid
- Botulinum toxin (Botox): These injections prevent the nerves that provoke sweat glands. Several injections are needed for positive results.
- ETS (Endoscopic thoracic sympathectomy): Recommended only in chronic cases, in which other treatments do not respond. It cuts the nerves that carry messages to the sweat glands. Used to treat face, armpits, and hands hyperhidrosis, but not for feet due to the risk of permanent sensual dysfunction.
- Microwave Destruction: Tool used to destroy sweat glands causing least damage to other tissues.
Natural Remedies
- Armpit Shields: Pads used to protect clothing from perspiration.
- Antiperspirants: These sprays include aluminum chloride which hinders the sweat glands.
- Clothing: Cotton or loose clothing can help, but synthetic fibers like nylon can deteriorate the situation.
- Shoes: Synthetic or plastic can make the condition worse, but natural materials like leather and rubber are recommended.
- Socks: Made up of cotton are best to absorb the moisture.
Complications
- Warts: Abnormal skin growth due to HPV (Human papillomavirus)
- Nail Infections: Especially toenails
- Heat Rash: Itchy and a red skin rash that results in a prickling and stinging sensation. Heat rash appears when the sweat ducts get blocked, and sweat gets trapped under the skin.
- Bacterial Infections: Specifically around the hair follicles and within toes.
- Psychological Impact: Excessive sweating affects a person’s relationships, jobs, confidence level. Some people get depressed, socially withdrawn and stressed.
Foods That Checks Excessive Sweating
- Bananas
- Whey
- Sweet Potatoes
- Almonds
- Green Tea
- Oats
- Olive Oil
- Cheese and Dairy Products (Calcium-rich foods)
- Good ole-fashioned H20
- Water dense vegetables and fruits (Eggplant, cauliflower, red cabbage, Peppers, spinach, broccoli)
The post Hyperhidrosis | Causes, Symptoms, Diagnosis & Treatments appeared first on Prime Health Channel.
]]>The post Carbuncle | Pictures, Causes, Symptoms, Diagnosis & Treatment appeared first on Prime Health Channel.
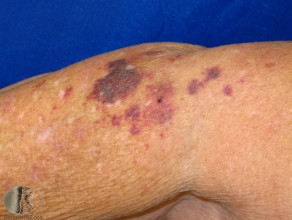
]]>Carbuncle is a skin infection that is characterized by red colored swollen and dome-shaped cluster of boils involving a group of hair follicles. The infection caused under the skin leads to formation of a lump which may damage deep through the skin and contain pus. It is also known as staph skin infection and usually grows to a size varying from 3 to 10 centimeters.
Occurrence of Carbuncles
Carbuncles are likely to occur on hairy areas of the body particularly at the back of the neck. But they may also be found on shoulders, thighs, groin, buttocks, and armpits. This can result in permanent scarring on the skin affected. They may be very painful if grown in closely attached surfaces like nose, fingers or ears. Carbuncles are very infectious too and may spread to other parts of the body and even to other people.
Comparison between Furuncles (boils) and Carbuncles
The staphylococcal infection causes Furuncles or skin abscesses and involves the hair follicles and adjacent tissues. They contain a limited amount of pus and when these furuncles or boils are connected subcutaneously and are clustered together, they cause deeper scars and more pus formation.
These are smaller and more superficial in nature. In comparison to boils, Carbuncles cause deeper and much severe infection accompanied by fever and chills. Carbunculosis is when there is more than one Carbuncle develops.
Symptoms of Carbuncles
- Painful red mass
- Appears as a nodule or a pustule
- Accompanied by fever or prostration
- Swift growth
- Center is white or yellow containing pus
- Weeping, oozing out or crusting of skin
- May spread to other areas
- Looks as small as a pea sized or as large as a golf ball
- Red and irritable on touching
- Fatigue
- Fever with high temperature of 38C (100.4F) or above
- Discomfort or feeling sick
- Itching skin on the affected area
- Swelling in surrounding tissues and lymph nodes
- Body ache
Causes for Carbuncles
- Infection by a notorious bacteria or virus (Primarily staphylococcus aureus bacteria)
- Bacterial infection entering through hair follicles
- Underlying condition of eczema or acne
- Previous amalgamation of boils
- Infection by microorganisms
- Folliculitis
- Rashes caused due to harsh shaves
- Hair pulling
- Poor nutrition
- Immune deficiency
- Poor hygienic conditions
Risk factors for Carbuncles
Although everyone bears the risk of developing Carbuncles, some factors may increase the risks of its occurrence:
- Old age
- Obesity
- Poor hygienic conditions
- Overall poor health
- Chronic skin conditions
- Diabetes mellitus
- Kidney disorders
- Liver problems
- Weak immune system
- Sharing bed linens, towels or clothing of others
- Wearing tight clothes
- Shaving and other activities breaking the skin
- Insect bites on the skin with heavy perspiration
- Acne and eczema patients
- Neutrophil disorders
- Living in crowded quarters
- Contact with virulent strain infected people
- Close contact with Carbuncle affected people
- Dermatitis
- Side effects of Immune modulating agents
Complications of Carbuncles
There might be severe complications related to these boils or Carbuncles. Sometimes, methicillin-resistant Staphylococcus aureus (MRSA) bacteria cause Carbuncles and the lesions must be drained out properly through high dosage of antibiotics to prevent further damage. Some of the common complications have been discussed below:
- Sepsis
- Infections in different body parts
- Lung infection
- Bone infection such as osteomyelitis and joint damage
- Infections in blood
- Heart disorders like endocarditis
- Effect on central nervous system
- Cellulitis infecting deeper sections of skin
- Permanent scarring
Diagnosis for Carbuncles
- Doctor can easily detect Carbuncles by merely looking at the affected area
- Pus sample is needed for lab analysis
- Span of the Carbuncle if lasts for two weeks
- Lesion culture
- Urine test
- Blood tests
- Clinical evaluation
Treatment for Carbuncles
Usually, Carbuncles or simple boils can be treated with home methods. But if chronic, the doctor’s recommendations are crucial. One must never take the risk to drain a Carbuncle by him as it can lead to infections in the bloodstream. Some common treatments and medicines that doctors might prescribe are:
- Oral Antistaphylococcal antibiotics for healing severe cases
- Trimethoprim, sulfamethoxazole, clindamycin, and doxycycline or minocycline
- Incision at the tip of the Carbuncle and drain out the pus
- Deep Carbuncles require sterile gauze to soak and get rid of the additional discharge of the pus
- At times, antibiotic ointments rubbed onto the skin also helps to heal
- Painkillers may be used for reducing pain
- In extreme cases for deep and large Carbuncles, they need to be operated after draining it out.
- Antibacterial soaps also prescribed by the doctors to be used daily
Home remedies for treating Carbuncles
- Warm compressing over the Carbuncle
- Soak the Carbuncle in warm water
- Application of clean, warm moist cloth for 20 minutes at frequent intervals in a day
- Apply heating pad or a hot water bottle for 20 minutes many times a day
- After every use clothes and wraps must be washed in hot water to be freed of germs
- Covering the area with sterile bandage
- Medications such as Acetaminophen or Ibuprofen relieve the pain
- Use of over-the-counter painkillers such as paracetamol or ibuprofen to reduce pain
- Cleanse skin with antibacterial soap
- Apply soap and wash your hands with warm water after touching a Carbuncle or the area
- Prevent contamination
- Never squeeze a boil or leave it open
- Bandages worn should be changed at regular intervals and thrown in closed bags
Prevention of Carbuncles
Carbuncles or infected boils cannot always be avoided but some measures must be adopted and proper hygiene must be maintained to reduce the risk of its occurrence:
- Clean the skin using a mild antibacterial soap
- Clean the cuts, wounds and injuries very carefully
- Cover the wounds and cut with sterile bandages until they get entirely healed
- Healthy diet and regular exercise helps to boost the immunity system
- Clean hands before eating and after using the bathroom
- Have frequent showers to free the skin from bacteria
- Avoid squeezing of boils and rubbing of broken skin
- Use of cleansers with chlorhexidine, triclosan, and triclocarban in them
When to call a doctor?
Typically, boils and Carbuncles do not require medical treatment as they tend to burst and heal by themselves. If the Carbuncle is lying somewhere adjacent to the nose, spinal cord or eyes, one must call the doctor immediately or else it can lead to severe problems. But there are certain conditions if noticed and then you must consult a doctor:
- Carbuncles on nose, face or spinal cord
- Carbuncles extremely painful
- Carbuncle which grows bigger when touched feels soft and spongy
- Those which do not heal within two weeks
- High temperature & chills associated with the boils
- Feeling unwell
- Recurrence of the Carbuncles
- Prolonged lasting of the lesions
- Weakness & exhaustion
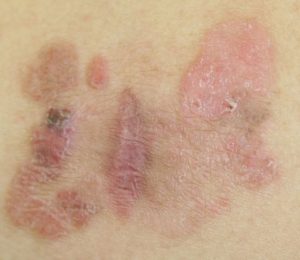
Carbuncles Images
The post Carbuncle | Pictures, Causes, Symptoms, Diagnosis & Treatment appeared first on Prime Health Channel.
]]>The post Senile Purpura appeared first on Prime Health Channel.
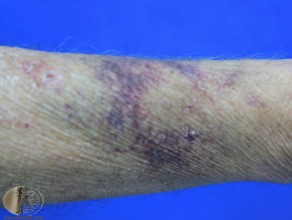
]]>Senile Purpura also termed as actinic purpura is a common skin condition that is benign and causes bruises, particularly on forearms and legs. They can also occur in the mucous membranes, especially in the mouth or other internal organs. They are largely common in old people as their skin as well as blood vessels becomes very fragile and thin.
Characteristics of Senile Purpura
In initial stages, they are purplish red and appear as patches or spots on the skin. They may also be called as skin hemorrhages or blood spots. Varying in size, large purpura spots are called ecchymosis while the smaller ones are termed as petechiae.
They do not occur from any deficiency of vitamins or minerals, neither because of any bleeding disorders. Not only severe trauma, but even mild traumas can also lead to the development of these bruises. They are formed when blood leaks under the skin or at the joints of blood vessels.
Causes of Senile Purpura
Some may have the opinion that senile purpura is the effect of vitamin and mineral deficiency, but this is not at all true. The underlying causes are mentioned below:
- Aging
- Too much exposure to the sun
- Overuse of blood-thinning medicines like steroids & aspirin
- Vascular disorders
- Diabetes
- High blood sugar levels
- Thrombocytopenia (deficiency of platelets)
- Blood clotting diseases
- Inflammation of blood vessels
- Changes in pressure during childbirth
- Haemangioma
- Amyloidosis
- Medicines affecting platelet functions
- Meningococcemia
- Infection in brain & spinal cord
- Blood infections
- Bacterial reactions
- Rheumatoid arthritis
- Lupus
- Various drugs like corticosteroids
- Minor trauma
- Connective tissue diseases
- Scurvy
Occurrence
The disorder of senile purpura occurs mostly in older people. About 10% of the people over the age of 50 years get affected by this. This percentage rises with age as More the age; more the people will be prone to this skin disorder.
Symptoms of Senile Purpura
Common senile purpura symptoms appear such as:
- Thinning of skin
- Skin tears very easily
- Large purplish red bruises
- Irregularly shaped lesions from 1-4 cm
- Dark colored lesions on hands, forearm, face & neck
- Adjacent skin inelastic and thin
- Bruises disappearing in three weeks
- Brown or yellow discoloration on fading
- Bruises occur with or without trauma
- Unchanged bruise color till disappearing
- Occurrence in chronic relapsing conditions
- Brown patches remain permanent on skin
Diagnosis for Senile Purpura
It is really important to diagnose senile purpura. The doctor studies all symptoms and medical history of the patient and also undergoes a physical test. He would carry out a thorough examination of the patient. Some tests needed to diagnose the condition are:
- Capillary fragility test
- Bean arm test
- Skin atrophy
- Platelet examination
- Hemostasis tests
- CBC (complete blood count test)
- PT, PTT with INR (a coagulation profile)
- Urine test
- Liver function test
- ESR or CRP test
- Renal function tests
- Skin and blood culture test
- Rheumatoid factor test
Differential diagnosis of Senile Purpura
Again diagnosis may be carried out in different ways for different types of senile purpura. The two types are:
- Palpable purpura
- Non-palpable purpura
Palpable purpura diagnostic measures include detection of:
- Rheumatoid arthritis
- Systemic lupus erythematosus
- Sjogren’s syndrome
- Malignant Lymphoma
- Multiple myeloma
- Leukemia
- Vasculitic injury in liver, kidneys, brain, lungs or gastrointestinal tract
- Blood abnormalities & any infection
- Check if nay intake of reacting drug
- Polyarteritis nodosa
- Henoch-Schonlein syndrome
- Granulomatous vasculitis
- Detect if infusion of drugs like heparin, warfarin, NSAIDs & aspirin,
Non-Palpable purpura diagnostic measures include detection of:
- Dissemination of intravascular coagulation
- Thrombocytopenic purpura
- Thrombocytopenia by drug induction
- Idiopathic thrombocytopenic purpura
- Bacteremia
- Viral infected diseases
- Scurvy
- Chronic statis
- Trauma
- Torch infection
- Systemic disorders
- Anticoagulation therapy
- Actinic variation in body
Diagnostic tests for both these types include:
Conditions for Diagnosis
- Typical in elderly (male and female) more than 60 years of age
- Regular platelet count
- Skin purpura of 1-4 cm diameter mainly on hands, legs, face, neck & underarms
- Positive beam arm test
- Skin atrophy of the affected area
- Normal hemostasis
Treatment for Senile Purpura
The disorder is considered harmless and fades away with time. However, people may not like these patches or bruises on their skin so many seek treatment, which may include:
- Supplementation with vitamin C
- Intake of flavonoids and antioxidants
- Retinoid for further prevention
- Wearing guards on limbs for protection of trauma or injury
- Citrus bioflavonoids twice a day
- Use of tretinoin
- Laser therapy
- Application of topical vitamin K after laser therapy to minimize bruising
Complications of Senile Purpura
Senile purpura does not have any serious complications as it is a benign condition. Only the lesions erupted on the skin may be emotionally distressful and irritating to the patients because it creates a cosmetic disfigurement of the skin.
When to Visit a Doctor?
Senile purpura although harmless, if left untreated may be recurring in occurrence. Using sun blocks and other protective measures can prevent further damage to the skin.
Mostly, purpuric eruptions may last from a week and can extend up to three weeks or so. However, the discoloration might be permanent even after the lesions fade away causing a brown patch in the affected area. One should immediately consult a dermatologist to reduce their appearance.
Prevention for Senile Purpura
- Lifelong usage of sun protection
- Avoid exposure to the sunrays
- Avoid getting out in the sun during 10 am to 3 pm
- If outdoors, wear covering clothes for protection
- Apply sunscreen lotions to the exposed parts of the body
Senile Purpura Pictures
The post Senile Purpura appeared first on Prime Health Channel.
]]>The post Maculopapular Rash | Picturtes, Causes, Symptoms, Diagnosis & Treatment appeared first on Prime Health Channel.
]]>Macules are a small, flat, non-elevated and discolored area on the skin. Usually, macular rashes do not require any treatment initially, but in case it continues for more than two weeks, a doctor needs to be consulted. On the other hand, papules are small swollen bumps on the skin. Papules are also known as HIV rash.
What is Maculopapular Rash?
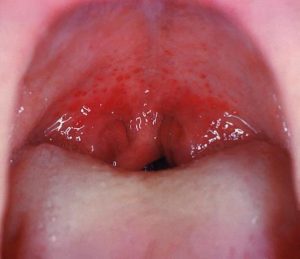
A maculopapular rash is a skin condition in the form of macules or papules or both. Termed as maculopapular with the fusion of the two words, they are tiny red spots that are found in different areas of the skin. These raised patches appear due to several medical reactions and infections like Measles, Scabies and Syphilis which normally occurs when the immune system gets weakened.
Characteristics of a Maculopapular Rash
The rashes often lead to the growth of tiny inflammations on the skin in the form of lumps commonly found on the hands and feet. They may be both flat and elevated lesions appearing on the skin that tends to merge. If these rashes develop larger than 1 cm in size, they are then considered as patches. But if they are merged, then it is a plaque.
Incidence of Maculopapular Rash
They are found in acute, less advanced and chronic stages.
- Acute cases last less than a month
- Subacute conditions may last for one to two months.
- Chronic cases these rashes may stay for more than eight weeks.
Maculopapular rashes are common in all age groups and may develop at any part of the body, be it the trunk, face or any other area. Adults mostly suffer due to the side effects of certain drugs and allergic reactions. On the contrary, children suffering from viral infections are prone to get these rashes on their palms and soles of feet. In earlier stages, they may be red but gradually develop discoloration.
Causes of Maculopapular Rash
A maculopapular rash may occur due to several disorders:
- Reaction to drugs: An intake of several medicines such as antibiotics, anticonvulsants, Cefobid. Cefoperazone sodium, etc. for a prolonged time may cause allergic reactions. A low fever and muscle pain may accompany these rashes but would fade away in a week or two.
- Epstein Barr Virus: A virus infection leading to painful eruptions on the skin along with fever is common among cancer patients mainly in China and Africa.
- Syphilis: People infected with Syphilis which is a sexually transmitted disease may develop these rashes on their genital organs which can be quite itchy and painful.
- Scabies: Infections caused by itch mites is known as Scabies and may cause serious itching anywhere on the body.
- Rubella: German measles termed as Rubella may also be a reason.
- Chikungunya: Maculopapular rashes accompanied with high fever and joint pain can be caused due to Chikungunya.
- Dengue: Patients suffering from dengue due to mosquitoes can be infected by fever, rashes, joint pain and even a drop in the platelet count.
- HIV: AIDS primarily caused by the HIV can also contribute towards these rashes.
Other possible reasons
- Dropping levels of Cholesterol
- Autoimmune responses to certain intakes or the body’s systematic inflammation
- Infections such as EBV infection, measles, scarlet fever, herpes, Ebola, hepatitis B or C, etc.
- Insect Bites
- Unusually high exposure to sunlight
Symptoms of Maculopapular Rashes
In the initial stages, rashes are red and bright in color accompanied with small structures that gradually get discolored. They are often accompanied with:
- High fever, fatigue, throat pain in case they are due to measles
- Tendency of vomiting
- Headaches may accompany the rashes
- Difficulty in breathing
- Skin becomes rough and dry
- Pain in the muscles
- In case of meningococcemia being the reason, joint swelling and pain are symptoms
Diagnosis of Maculopapular Rash
Diagnosing the rash may take some time and can be quite difficult as there are several potential causes. The following are the steps taken to the doctor for a diagnosis:
- Assessing the patient’s medical history about the past ailments and the causes
- Careful inspection of the rashes and the affected area through microscopy
- Occurrence of itchiness, pain and irritation on the affected skin should also be noted
- Cerebrospinal test and even a syphilis test for appropriate detection
- Blood count test, a blood culture test to verify if any virus or bacteria has invaded the body
- ENT examination and tests of the lungs, genital organs, muscular joints, and nerves may also be conducted
- Check for associated symptoms like Measles
- Rashes accompanied with a headache could be due to Gonococcemia
- Urine test may also be suggested by the doctor to check the presence of virus or bacterial infection
- Skin biopsy might also be needed
Treatment for Maculopapular Rashes
The actual treatment lies in the detection of the underlying disease, finding out the notable symptoms and reducing the irritation and skin rash. Experts will find out the original disorder due to which these eruptions occur and try to curb down the main disease by reducing the symptoms too. The following are some treatments depending on the symptoms:
- Chloroquine is usually recommended to control inflammation and itchiness if the causative agent is the Chikungunya virus
- In case of dengue, Intravenous fluids are given, and in serious conditions of Dengue infection where platelets fall remarkably, blood transfusion is needed
- Painkillers are prescribed in case of EP virus infection
- Intake of plenty of fluids and hydration of the body is required
- In chronic cases, ultraviolet radiation might be helpful
- If several drugs or medicines are a cause, then the only way is discontinuation of its usage
- Adequate rest along with antibiotics, antiviral, oral hydration and IV infusions are advised to prevent it from infection
- Use of topical corticosteroids and oral antihistamines may redeem the condition
Other Treatments for Maculopapular rashes
- Certain topical ointments may help in eliminating the rash and provide immediate relief
- Loose clothes should be used to reduce the swelling and pain
- Have baths using baking soda
Complications related to Maculopapular rashes
One major complication linked to this is the Zika virus. It can affect the baby even if the mother has had mild symptoms of the disease. It can cause an underdeveloped head in the baby of the mother affected with the Maculopapular rash caused by Zika virus during the initial months of pregnancy. Hence, one should check up with the doctor during pregnancy to detect if she has got any exposure to the Zika virus which is a sexually transmitted disease or born by mosquitoes.
Maculopapular rashes Pictures
The post Maculopapular Rash | Picturtes, Causes, Symptoms, Diagnosis & Treatment appeared first on Prime Health Channel.
]]>The post Petechiae | Pictures, Characteristics, Causes, Symptoms, Diagnosis & Treatments appeared first on Prime Health Channel.
]]>Petechiae are round, pinpoint spots that appear on the surface of the skin due to minor or major health conditions. These spots are a result of breaking of blood vessels known as capillaries which cause blood to leak into the skin.
Petechiae often occur in clusters; hence people also refer to them as petechial rashes. However, they are not rashes but spots that occur due to bleeding under the skin. The difference lies in the fact that petechiae are flat to touch and do not lose color on application of pressure on, them, while a rash loses color under the same circumstances and they feel uneven.
Characteristics
- Location: They can appear in any part of the body. However, they commonly occur on the face, back, thighs, ankles, shoulders and neck.
- Color: The spots are red in the initial stage, but they change color They then turn purplish or bluish, and at the end, the color becomes dark purple or blue.
- Size: Its size is not more than 3mm and they measure from 0.5 to 1mm in diameter. Petechiae that measure more than 3mm are called purpura.
- Fading: Applying pressure does not cause petechiae to lose color; this is what differentiates them from rashes.
Causes
- Straining: Prolonged straining due to activities such as coughing, weight lifting, childbirth, vomiting, crying, etc. may result in the appearance of tiny petechiae on the neck, face and chest. Such conditions are a result of the excessive pressure that causes the breaking of the capillaries.
- Medication: Certain medications react on the body in a way that causes spots to appear on the skin. Medicines like anticoagulants, chloral hydrate, naproxen, quinine, nitrofurantoin, penicillin, desipramine, indomethacin, carbamazepine, atropine, etc. There is also a high possibility of petechiae occurring in people who may be allergic to some medicines.
- Infectious Diseases: Viral, bacterial or fungal infections can also result in petechiae. Such diseases include strep throat, viral hemorrhagic fever, scarlet fever, cytomegalovirus infection, meningococcemia, mononucleosis, Hantavirus pulmonary syndrome; Rocky Mountain spotted fever, sepsis, etc.
- Sunburn and Injuries: Individuals who sustain injuries after a crash or accident may develop petechiae. Similar spots may also appear on the face and eyes in case of child abuse or other physical abuse that includes smothering, biting, spanking, strangulation, etc. Similar reactions on the skin can also occur in case of severe sunburn.
- Vasculitis: It refers to a condition in which causes the walls of the blood to thicken, thus reducing the passage of blood flow and increasing pressure within the vessels. This pressure could result in the damage of these vessels and leakage of blood under the skin.
- Thrombocytopenia: In this condition, the body produces less blood platelet. These platelets colorless and are responsible for the clotting of blood. A decrease in the platelets will not allow the formation of plugs or clots that stop the bleeding from blood vessel injuries. This condition may further lead to petechiae.
- Leukemia: A type of cancer, the blood-forming tissues that decrease the body’s ability to fight infections. Less blood in the body may cause a strain and diseases can affect the system quickly.
- Deficiency: Vitamin K is vital for the formation of blood clots wherein a lack of this vitamin may cause petechiae. Scurvy is a disease that develops due to a deficiency of vitamin C. Absence of this vitamin in adequate amounts may lead to weakness, fatigue, rash, bleeding, bruising, etc. that are in close association with petechiae.
Symptoms
- Fever
- Malaise
- Flu-like symptoms
- Appearance of red spots on the skin that change color with the passage of time
- Spots are flat
Diagnosis
- Physical examination
- Thorough checking of the medical history
- Checking the platelet count
- Complete blood count
- Partial thromboplastin time
- Bleeding time
- Thromboplastin time
Complications
- Heart problems
- Damage to liver, spleen, kidneys, lungs, heart & other organs
- Infections in other parts of the body
Prevention
The following measures should be taken up to avoid petechiae due to infection:
- Keep your hands clean by using an alcohol-based hand sanitizer or wash them with soap and water
- Keep counter tops and other common surfaces clean
- Have safe sex
- Do not share personal items like glasses, utensils, towels, etc.
- Stay away from people who are sick or have an infection
- Use insect repellents while going outdoors, especially grassy or wooded areas and wear full sleeves and long pants
Treatments
- Antibiotics: Doctors prescribe antibiotics to patients for whom infection leads to petechiae. The medication not only reduces the symptoms of the infection but also helps to treat the infection itself. Once, the infection is over, the visible signs of petechiae also disappear.
- Platelet transfusion: Low platelet count may be the cause of petechiae in some cases. Platelet transfusion will help to increase the platelet count in the system, thus rectifying the problem of the appearance of the red spots on the skin.
- Withdrawal: Certain medications have an allergic reaction towards the body leading to the development of petechiae. If the individual or the doctor can identify the medication that is causing this reaction, then it is best to discontinue the use of that medication. A doctor’s suggestion is imperative in such a case so that he/she can suggest an alternative medicine.
- Cold compress: Use of cold compress in the area that has visible signs of injury to blood capillaries can help to treat the condition. Ice will help to recover from the damage and make the red spots disappear. Caution must be taken to place a cloth between the ice and the skin to avoid causing damage to the skin due to direct contact.
When to Visit a Doctor?
Consulting a doctor is necessary if the patient observes the following symptoms:
- Confusion
- High fever
- Trouble while breathing
- Change in consciousness
Petechiae Pictures
The post Petechiae | Pictures, Characteristics, Causes, Symptoms, Diagnosis & Treatments appeared first on Prime Health Channel.
]]>The post Erythema Marginatum | Pictures, Causes, Signs & symptoms, Treatment appeared first on Prime Health Channel.
]]>Erythema Marginatum is a rare skin disease usually accompanied by rheumatic fever caused due to bacterial infection. It causes rashes marked by pink or red circle patches. Erythema meaning red and Marginatum is the Latin form of the English term ‘margin’. So signified by its name, the margins of these ring-like rashes remain visible, the center remains flattened, and the reddened edges are elevated.
How long does Erythema Marginatum last and what are its characteristics?
It may last for months which appear and disappear and again reappear over the course of several months. These reddish circles are mainly results of allergic reactions caused by various drugs, chemicals, or may occur due to some unknown reason. They are prevalent in the trunk, mostly the upper portion of the body, inner regions of arms and limbs and primarily seen on the surface underlying the extensor muscles. However, the face, palms, and soles of feet are not affected in maximum cases. But an issue with this they go unnoticed as they are neither painful nor itchy. Hence, in most cases, it gets ignored.
Types of Erythema marginatum
Erythema Marginatum is mainly of two categories:
- Erythema marginatum rheumatism is the type that is accompanied by rheumatic fever and develops on the trunk and seen on the inner surfaces of the limbs. It occurs as multiple eruptions and spreads all over, but is superficial in occurrence.
- Chronic Erythema Marginatum perstans develops in the deeper areas of the body apart from the palms of hands and soles of feet. Their growth is in the form of lesions and distributed throughout the surface of the skin. This category reappears on frequent periods and erupts on a permanent basis.
Erythema Marginatum affects mostly light-skinned people. It is commonly found more in males than in females and can affect people of all ages. These rash circles measure about 0.5-2 centimeters in diameter and are spread out eruptions on the body.
Causes of Erythema Marginatum?
Several causes can trigger these eruptions. Among the possible causes, rheumatic fever is considered as the most common factor for Erythema Marginatum. Some of the common causes are:
- Rheumatic fever: Streptococcus pyogenes is the affecting bacteria that cause this disorder. Ring-like structures are produced on the skin and they affect the heart, joints and even the brain. Acute high fever increases the risk of these projections and turns more serious. It is common in children in the age group of 5-15 years, but it can affect anyone. Being painless, they often go unnoticed and can reoccur within days or several months.
- Lyme disease: It is an infectious disease caused by Borrelia burgdorferi, a harmful pathogen that enters the human blood through infectious bites of ticks. It is found explicitly in North America.
- Hypersensitivity or allergic reaction: Extreme reaction or intolerance to the stimuli or other agents may produce this type of allergic outbursts on the skin. Mostly these are caused due to food allergies, particularly blue cheese and tomatoes are prominent in this case.
- Malignancy: Chronic ailments such as breast cancer, leukemia, lymphoma and several other life-threatening diseases may also cause these symptoms and produce rashes.
- Infection: Reactions caused due to various infections may also result in the onset of small red eruptions. Escherichia coli, Candida albicans or Ascaris lumbricoides are some of the infectious agents.
- Adverse reactions to drugs: Regular use of anti-malarial chloroquine or hydroxychloroquine, gold, penicillin, and cimetidine can be factors for these eruptions due to an adverse effect on the patient.
- Hormones: Pregnant women are more likely to suffer from this type due to hormonal changes. Also during the onset of puberty in children of 15 years or those who have already entered their puberty stage may suffer from Erythema Marginatum as they undergo a hormonal change.
Signs & symptoms of Erythema Marginatum
- Ring-like eruptions
- Slight elevation on the edges
- No presence on the face
- Red or light pink circular structures
- Found mainly on the torso and extremities
- No itching sensation
- Appearance like a smoke ring
- Eruptions turn pale when pressed
- Sharp well-marked edges
- Intensifies with heat and reduces with normal temperature
- Measures usually 0.5-2 centimeters in diameter
- Strep throat infection in some cases
- Intense pain in joints of knees and elbows.
- Tiredness
- Breathing problems
- Chest pain
- Extreme palpitations
- Inflammation in the heart and central nervous system
- Increases after a shower or exposure to sunlight
Diagnosis of Erythema Marginatum
The disorder can be diagnosed depending upon the accurate observation and examination of the skin conditions. Also, skin specialists should check the medical history of the patient which is equally necessary to check if any other disease can be the cause of this rash or any reaction to a drug or chemical.
A biopsy is often required to check if other acute disorders are associated with these eruptions. A small section is removed from the outermost layer of the skin for a biopsy.
Some of the other ways to diagnose the disease include:
- Blood test for complete blood count
- Throat swab to check for presence of Streptococcus pyogenes
- Electrocardiogram (ECG) to check if there is proper functioning of the valves & chambers of the heart
Similarity to other related disorders
This disorder can be confused with similar conditions like erythema nodosum, erythema migrans, and erythema multiforme.
Difference between Erythema Marginatum & Erythema Migrans
Erythema migrans may appear due to an infectious tick bite and can occur within a month after the bite. It is similar to Erythema Marginatum, but the only factor differentiating them is that the former has a bull’s eye appears in the middle of the eruption which is not present in the latter.
Difference between Erythema Marginatum and Erythema Multiforme
Erythema multiforme usually has a mild itching sensation, but in severe cases it is extreme. However, the rashes are non-itchy. Also in both the conditions, it varies in appearance.
The disorder also shows similar symptoms as of Hives or Urticaria, a disorder where the person is affected by red itchy elevated patches on the skin of different shapes and sizes. These are mainly caused due to drug reactions. But the major difference is that the rashes in Hives or Urticaria are not visible while itching.
Who are at risk?
Anyone, be it a child or an adult with rheumatic fever may suffer from this disorder. Reactions to chemicals, various drugs, poorly maintained sanitation facilities and several harmful environmental issues can increase the risk of infection by the strep bacteria.
Erythema Marginatum Complications
Erythema marginatum itself does not cause any complications, even if it lasts for weeks or months or even years together. However, it results in producing skin rashes and inflammation. Since it is not a disease in itself, it has no complications as such.
That being said, in a few cases, the soft membranes of the heart may be affected due to the decreased blood flow or leakage of the valves caused due to inflammation. However, the condition does not act fatally and is easily recovered by a proper diagnosis of the bacterial infection causing rheumatic fever. Intake of antibiotics for a prolonged treatment can help in preventing the repeated occurrences of fever.
However, patients with rheumatic fever can suffer from some of the below-mentioned diseases:
- Sydenham’s chorea
- Myocarditis
- Several cardiac disorders
- Subcutaneous nodules
- Polyarthritis
Good news is that experts are trying their utmost to invent a vaccine which would prevent rheumatic fever completely curing it, and as a result, the possibility of the occurrence of Erythema Marginatum can also be eliminated.
Treatment for Erythema Marginatum
In case the patient is diagnosed with rheumatic fever, treatment will be done accordingly to curb down the infection. For Erythema Marginatum associated with rheumatic fever, the below options may help to lessen the occurrence of severe rashes:
- Penicillin injections
- Benzathine benzylpenicillin to eradicate the bacteria
- Aspirin, Anaprox & other Salicylates to reduce pain & inflammation
- Corticosteroids & other Anti-inflammatory drugs
- In case of carditis Digoxin, ACE inhibitors, beta blockers, and diuretics
- Salicylates to reduce pain & fever
- Anticonvulsant drugs like valproic acid or carbamazepine
- Creams & ointments even moisturizers
But it must be kept in mind that certain drugs or medicines can worsen the condition. Also, avoid allergic foods which may trigger irritation.
When to call the doctor?
If the patient suffers from recurring rheumatic fever for three to five consecutive years, it is highly recommended to consult a doctor. If the valves and membranes of the heart get affected due to inflammation, it may lead to life-threatening diseases.
Erythema Marginatum Pictures
The post Erythema Marginatum | Pictures, Causes, Signs & symptoms, Treatment appeared first on Prime Health Channel.
]]>The post Subungual Melanoma appeared first on Prime Health Channel.
]]>Melanoma is a kind of skin cancer that begins to grow in the cells comprising of skin pigments called melanocytes. When melanocytes start to collect, it results in the formation of moles that may turn cancerous. In case Melanoma is not treated timely, cancer might spread to other organs. Melanoma usually occurs when an individual is exposed to the ultraviolet rays of the sun.
What is Subungual Melanoma?
Subungual Melanoma is a rare condition of Melanoma under the fingernails. Unlike other skin cancers, it occurs on the nail bed, known as the nail matrix, which helps in protecting the underlying skin. It causes the nail to discolor and is characterized by dark brown or purple color appearing as a streak of dark pigmentation that results in thinning and ultimately breakage of the nail. It is often seen on the big toe or thumbnail. However, it may occur in any nail of the foot or hand.
Subungual Melanoma Incidence
It is noted that 1% – 5% of all melanoma cases are of Subungual Melanoma affecting the fingernails of both males and females. It is most common in Asians and those of the African-American descent who are intensely pigmented. It is largely found in people within the age group of 60-70 years. It is however rarely seen in children. This form usually is non-malignant but if cancerous can prove harmful leading even to death.
Appearance of Subungual Melanoma
Although in a few cases, the nail might not face pigmentation, the early symptom is a streak of pigmentation on the nail bed. It is quite visible to the naked eye. During its development through the days, it appears like:
- Pigment turns first into light brown, purple or black
- Gradually spreads out and covers the closest nail fold
- Tends to become wider on the cuticle
Symptoms of Subungual Melanoma
In most cases, a dark patch appears underneath the nail. Many females may not be able to see the initial signs if they wear dark shades of nail paints. In its early development, it looks like a mole on the skin which is caused by the sun rays.
- Small lump under the nail without any color
- Dark purple, black or brown spot on the nail
- Blood from the nails but no pain
- Streak or band of light to dark brown color on the nail mostly vertical
- Dark brown or purple band tends to expand and slowly grow
- Pigmentation may also extend to the skin surrounding the nail
- Nodule underneath the nail with or without a pigmentation band
- Affected nail appears cracked, thin and brittle
- Bleeding along with the pigmentation
- Patches or the streaks on the nails
- Bruise on the nail that does not heal soon
- Nails of the finger or toes get separated from the nail bed
- Skin adhering to the nail gets darkened
- Nodule develops underneath the nail causing bleeding
- Nail bed gets distorted
- Split nails
- Painless bleeding of the cells in the nails
Causes of Subungual Melanoma
Primarily the reason for this disorder is cancer. Mainly three categories of cancer urge the occurrence of Subungal Melanoma-
- Acral lentiginous melanoma affects the nail matrix
- Desmoplastic Melanoma.
- Nodular melanoma.
Diagnosis of Subungal Melanoma
Diagnosing this form of cancer is difficult which is why it is highly recommended to consult a doctor immediately after noticing any patch or any unusual growth on the nails. The doctor needs to examine the region of the nail and the lesion carefully. Dermatologists may use an instrument called a dermascope which helps them to get a magnified view of the affected nail and its surrounding area.
But in a few cases, visual inspection may be harmful as it may be confused with other disorders like the subungual hematoma, onychomycosis.
The only technique for detection is a biopsy. Two procedures are:
- A biopsy is known as a punch biopsy is a tubular instrument containing a sharp end that acts like a cookie cutter that collects the sample. It enables the doctor to look for other fungal infections apart from melanoma.
- For advanced melanoma suspicion, the biopsy associated with the excision is undergone to remove the entire part of the nail along with its surrounding tissue.
Risk factors regarding Subungal Melanoma
People who prone to get affected by risk factors do not immediately get affected by this disease. But they bear the risk of suffering more than the ordinary ones. Hence they should be more careful with the early symptoms and readily visit a doctor.
Some of the common risk factors include:
- Exposure to direct sun and ultraviolet rays light for a prolonged period
- People having darker skin are more likely to suffer
- People aged above 50 are more at risk
- Medical history associated with trauma to the fingers or toes increases the risk
- Patients affected by HIV or other immunosuppressive disorders
- Genetic history of melanoma
- Occurrence of several moles
- Hereditary conditions of Xeroderma Pigmentosa (extreme sensitivity to UV radiation)
Complications caused by Subungal Melanoma
Similar to other cancers if not treated timely it can spread to other parts of the body. Melanoma affects other organs causing life risks. At times, the doctor may suggest an amputation to be done on the finger or the toe on which the nail gets pigmented. However, compared to this, surgery is more advisable.
Treatment for Subungal Melanoma
The preferred method to get rid of Subungal Melanoma is to adopt a surgery. The doctor firstly removes the entire nail affected and then it can help him to discard the cancer development thoroughly. But again, this depends on the intensity of the disorder verifying on what stage it is and how complicated can it get.
- Initially, if the depth is less than one millimeter, then the doctor usually undergoes local expurgation. It can help to control the development of cancer.
- In case, it is wider and dangerous, an excision is required along with the biopsy of the lymph node. It is needed to conduct the nature of the melanoma and reduce the risk of spreading to other organs through medications and proper methods.
- But if the melanoma is too advanced, then the affected finger or toe needs to be operated and removed. Thus all of the cancerous element presents can be expurgated entirely and thereby no further complications can arise.
- Unfortunately, if the surgery does not work, then the last option is to undergo chemotherapy and use of prescribed medicines to kill cancer in the cells of the affected area or anywhere surrounding it.
However, till date, the most viable option for the cure of this melanoma is surgery.
Pictures of Subungual Melanoma
The post Subungual Melanoma appeared first on Prime Health Channel.
]]>The post Bowen’s Disease appeared first on Prime Health Channel.
]]>Bowen’s disease is a rare, slow-growing, non-hereditary skin disorder, characterized by reddish, scaly patches. Named after physician JT Bowen, who discovered it in 1912, it is also referred to as squamous cell carcinoma in situ, indicating that it is an early stage of skin cancer. However, it has been estimated that amidst 100 patches of Bowen’s disease, only three may turn cancerous.
Signs and Symptoms
The most prominent symptom is a single scaly patch with an irregular outline, but there may be multiple patches too. There are some characteristics of these patches that help with initial detection:
Color: Reddish brown, pink or white
Size: Diameter may range from a few millimeters to several centimeters
Features: May bleed, ooze pus, itch, split open or become warty, crusted, delicate and darkly pigmented
Affected areas: Commonly affects the lower legs, arms, ears, face and neck. Less affected areas include the head, palms, anus, vulva, soles, scalp, lips as well as the area around nails and inside mouth. In young adults, the genitals are mostly affected.
Causes
The disorder occurs when the keratinocytes cells, present in the outer layer of the skin, grows abnormally fast, resulting in the flaky accumulation of dead skin cells. However, what exactly triggers such a sudden growth is not known. There are certain factors often associated with the occurrence of the disease.
Risk Factors
The disorder, more common in aged women than in men, is most likely to affect those who:
- Have a suppressed immune system due to medication or other medical ailments
- Are exposed to ultraviolet rays of the sun for long durations
- Are exposed to arsenic through food or medicine
- Have been infected with human papillomavirus (HPV)
- Are exposed to ionizing radiation
- Have a previous skin injury such as scarring
- Have inflammatory skin problems such as eczema
- Are suffering from some rare genetic disorder
Complications
- Internal malignancy
- Lung Cancer
Diagnosis and Tests
The diagnosis generally involves:
- Skin examinations to thoroughly evaluate the symptoms and rule out other skin problems
- Biopsy of the affected tissue to confirm the disease
Differential Diagnosis
- Actinic keratosis
- Basal cell carcinoma
- Squamous cell carcinoma
- Seborrhoeic keratosis
- Psoriasis
- Eczema
- Bowenoid papulosis
- Paget’s disease of the breast
- Lupus vulgaris
- Ringworm
Treatment and Management
There are different treatment measures available for this noncontiguous disorder; but first, the following factors are evaluated.
- The size and thickness of the lesion
- The number and location of the patches
- Age, general health, and ability of the affected person
Treatment Options for Small Lesions
SurgeryThis is executed by removing the affected skin patch of areas such as the genitals.
Topical Application of Creams
Chemotherapy creams such as 5-fluorouracil (5-FU) and imiquimod applied directly on the lesion, once or twice daily for about two weeks, may help in eliminating the abnormal cells, and slowing down their growth. However, both may have side effects such as redness and inflammation which may require the application of a mild steroid cream like Fucibet.
Curettage and Electrocautery
After giving a local anesthetic, the concerned patch is scraped away, and electricity or heat is then employed to stop any bleeding that occurs and to remove any existing abnormal cell. A scab that develops afterward naturally falls off within a few weeks.
Treatment Procedures for Large Lesions
Photodynamic Therapy (PDT)
A short procedure lasting for about 20‑45 minutes, it is carried out by applying a light sensitive cream on the affected area before directing a light source to activate certain chemicals in the cream, which then burn the abnormal cells. The side effects comprise of a stinging or burning sensation that goes away within a few weeks.
Cryotherapy
Done by spraying liquid nitrogen on the patches to freeze them, this procedure may leave the skin feeling cold and uncomfortable for some days. A scab that appears after a few days generally falls off, thereby removing the affected patch.
Mohs SurgeryIn this surgical excision, the edges of the lesion are traced using a microscope to remove only the cancerous tissues, while the surrounding healthy tissue is left undisturbed. Having the highest cure rate amidst all the treatment procedures mentioned here, it is usually carried out in case of large, recurrent lesions or in areas such as around the nail that need maximum preservation of its tissues.
Investigational Therapies
Radiotherapy and Laser Treatment
Laser therapy utilizes intense light to eliminate the affected tissues from small areas such as a finger. In radiotherapy, X-rays or grenz ray radiation is given if there are multiple patches to treat. However, these procedures are not widely employed and more research needs to be done to prove their effectiveness in the long run.
Can Bowen’s Disease be Prevented
It can be prevented by following appropriate measures like:
- Avoiding prolonged exposure to direct sun rays
- Always applying sunscreen when going outside
- Using safe tanning options like cosmetic bronzers
- Wearing protective clothing
Prognosis and life Expectancy
Bowen’s disease has a considerably high survival rate when taken care of properly at an early stage. However, if left untreated, it may progress to a life threatening invasive squamous cell carcinoma in 3% to 5% of patients. Hence, it is vital to have regular follow-ups with a certified dermatologist to detect signs of recurrence, which occurs in 1 out of 10 cases.
Bowen’s Disease ICD-9-CM Codes and ICD-10-CM Codes
The ICD-9-CM code of Bowen’s Disease is 230 234 and ICD-10-CM code is D04 (ILDS D04.L10)
The post Bowen’s Disease appeared first on Prime Health Channel.
]]>The post Behcet’s Disease appeared first on Prime Health Channel.
]]>Behcet’s disease or Behcet’s (pronounced: beh-CHETS) syndrome, named after the Turkish dermatologist Hulusi Behcet, is a rare inflammatory disorder that can affect blood vessels throughout the body. The autoimmune disease may cause inflammation in the eyes, sores in the mouth, ulcers on the genitals, and skin rashes, although the effects usually vary from person-to-person.
Causes
Behcet’s disease is not well understood, and more research is needed to establish its specific causes. However, some research works indicate that bacterial, viral, environmental, and genetic factors play a role in causing the immune system to attack its own healthy blood vessels and cells. Exposure to infectious agents like Staphylococcus, Escherichia coli, Streptococcus bacteria, and herpes simplex virus could possibly trigger its development in individuals who are genetically susceptible to the disease.
Risk Factors
- Gender: Men are more likely to get affected than women.
- Age: Occurs usually in both young and middle-aged men and women (20-40 years old), although children and older people also can have Behcet’s syndrome.
- Origin: It normally affects people from countries along the old Silk Road, stretching from the Far East to the Middle East, including Japan, China, Iran, Egypt, Israel, and Turkey.
- Genes: People with the gene HLA-B51 or HLA-B5 are at risk of developing the disease.
Signs and Symptoms
Patients with Paget’s syndrome may experience episodes of the symptoms flaring up and getting better on their own (remission). Common symptoms include:
- Painful genital and mouth sores.
- Skin lesions such as acne-like spots or an abnormal growth.
- Lymphadenopathy causing abnormal enlargement or swelling of lymph nodes.
- Inflammation in the eye, called uveitis causes pain, redness, along with blurred vision.
- Pain and swelling of joints, involving knees, elbows, ankles, or wrists.
- Inflammation in veins and arteries causes pain, swelling, and redness in the arms and legs, which may result in the formation of blood clots.
- Systemic vasculitis may cause extreme fatigue, limiting the ability to do any activity and impairing quality of life.
- Abdominal pain, loss of appetite, indigestion, diarrhea, vomiting.
- A headache, loss of balance, fever, seizures, or double vision caused by inflammation in the central nervous system (CNS).
Complications
- Decreased or permanent loss of vision caused by severe uveitis.
- Bloody stools due to the damage caused by inflammation of the internal intestinal lining.
- Severe neurological disorders such as personality or behavioral changes, or partial paralysis due to CNS inflammation and brain stem lesions.
- Cerebral venous thrombosis or a blood clot inside the veins and arteries of the brain, increasing the pressure and cutting the blood supply, resulting in stroke-like symptoms.
- Aneurysms and blockage of blood vessels due to swelling in large arteries.
- Rarely, organ dysfunction or internal bleeding.
Diagnosis and Tests
No specific tests can definitively reveal Behcet’s syndrome since it takes several months or years before the common symptoms appear. Diagnosis is based on a set of clinical guidelines associated with the occurrence of symptoms.
The clinical criteria established for classification of Behcet’s disease states patients must have recurrent mouth ulcerations (thrice or more in a year) along with at least two of the following:
- Recurrent genital sores
- Retinal inflammation, uveitis, or other eye problems
- Skin sores and rashes
- Positive pathergy test
Imaging Tests
- Radiographs, MRI, or CT scan of sacroiliac joint and peripheral joints may indicate inflammation and accumulation of synovial fluid in the cavity.
- Brain MRI, CT scanning, or MRA to identify inflammation of blood vessels in the brain (cerebral vasculopathy) and places of restricted blood circulation (acute ischemia). SPECT scan (single-photon emission computed tomography) of the brain can indicate insufficient blood flow (cerebral hypoperfusion or ischemia).
- Angiography for evaluating aneurysms.
- Doppler ultrasonography to rule out other causes of venous blockage.
Pathergy Test
The patient’s forearm is pricked with a small, sterile needle and the area is examined after 1-2 days. The test gives a positive result if a small red spot or bump appears under the skin, which means the patient’s immune system has overreacted to the minor injury.
Other Tests
Bowel tests, lumbar puncture, and skin biopsy might be required for individual patients depending upon the symptoms for the diagnosis.
Differential Diagnosis
- Antiphospholipid Syndrome
- AA (Inflammatory) Amyloidosis
- Granulomatosis with Polyangiitis
- Paraneoplastic Syndromes
- Inflammatory Bowel Disease
- Systemic Lupus Erythematosus (SLE)
- MAGIC or “mouth and genital ulcers with inflamed cartilage” syndrome
- PFAPA or “periodic fever, aphthous-stomatitis, pharyngitis, adenitis” syndrome
- Reactive arthritis, psoriatic arthritis, ankylosing spondylitis
- Sarcoidosis
- HIV/AIDS
- Bacterial and viral infections
- Nutritional/hematological deficiencies
Treatment and Management
There is no cure for Behcet’s syndrome, though a treatment plan involving a combination of medications can help in relieving symptoms. Depending on the severity of symptoms, patients may need to take temporary medication to control flare-ups in pain and inflammation. Alternatively, people with Behcet’s disease may require long-term treatment to stop the development of serious complications.
Medication
- Corticosteroids like methylprednisolone, prednisone, and dexamethasone are given intravenously for arthritis, topically for ulceration or eye problems, and orally for systemic symptoms. Their long-term use may increase the risks of high blood pressure, heartburn, weight gain, and osteoporosis.
- Immunosuppressants including azathioprine, cyclophosphamide, chlorambucil, cyclosporine, and methotrexate to reduce the immune response, and thus stop the inflammation process that triggers other symptoms of Behcet’s syndrome. While mild side effects include hair loss, abdominal pain, and weakness, chronic use of these medications may cause liver and kidney function impairment. Some of the immunosuppressants may cause miscarriage or birth defects and should be avoided during pregnancy.
- Anti-inflammatory medication such as colchicine, triptans, and NSAIDs are used for lessening pain and headaches.
- Biologics like TNF-α inhibitors that target the antibodies associated with the process of inflammation. Common anti-TNF drugs include infliximab, interferon alpha, etanercept, certolizumab, adalimumab, and golimumab.
Surgery
Surgical care is needed when eye, lung, heart, gastrointestinal, and neurological complications develop, including:
- Abnormal narrowing (stenosis) in blood vessels of the intestine.
- Fistula formation, severe bleeding, and perforation in GI tract.
- Aneurysms and ischemic damage to the lungs, requiring surgical excision.
- Obstruction of blood flow in coronary arteries or veins (coronary thrombosis), formation excess tissues in endocardium (endocardial fibrosis).
- Sores and ulcers, not responding to medication.
- Cataracts, retinal detachment, and glaucoma.
- Aneurysms and clots in the central nervous system.
Alternative Methods of Management
- Activity level should be adjusted as tolerated by the patient. Some limitations are imposed if there are symptoms of arthritis present.
- Essential oils derived from cinnamon leaf, ginger, juniper berries, cypress, and clary sage may be used as anti-inflammatory massage oil for lessening joint pain and muscle stiffness.
Diet to Follow with Behcet’s Syndrome
Patients with Behcet’s disease involving gastrointestinal complications are recommended to follow a similar diet recommended for people with inflammatory bowel disease. Special liquid food containing glucose, salts, vitamins, minerals, lipids, and amino acids may be given intravenously. Anyone with the Behcet’s syndrome should avoid milk, cheese, ice cream, and yogurt since a recent study has shown intake of dairy products may worsen autoimmune symptoms in some individuals.
Prognosis
As medical therapy can relieve moderate symptoms and control flare-ups, patients with Behcet’s syndrome can lead a normal life. Deaths are occasionally reported in people exhibiting major vascular, gastrointestinal, or neurological complications, and frequent flare-ups.
Incidence and Prevalence
Data from recent studies in the US identified 0.12-0.33 cases of Behcet’s disease per 100,000 Americans. In Turkey, its prevalence is the highest being 420 per 100,000 population. It ranges from 13.5-22 per 100,000 inhabitants in Korea, Japan, China, Saudi Arabia, and Iran. In Europe and North America, only 1 case was reported per 15,000-50,000 inhabitants.
ICD-9-CM and ICD-10-CM Codes
The ICD-9-CM code for Behcet’s disease is 136.1, and the ICD-10 code is M35.2.
The post Behcet’s Disease appeared first on Prime Health Channel.
]]>The post Pemphigus vulgaris appeared first on Prime Health Channel.
]]>Pemphigus vulgaris (PV) is an autoimmune disease (condition in which the immune system turns against the body itself) characterized by the development of sores and blisters on the skin and mucus membranes [1].
Pemphigus vulgaris Epidemiology
This is a rare disorder having an estimated prevalence of 3.2 in every 100,000 population [2]. It is extremely rare during pregnancy [8] and in children. Males and females are affected equally.
Pemphigus vulgaris Signs and Symptoms
Around half of all sufferers first develop painful sores and blisters in the mouth. This is followed by the development of skin blisters. Skin sores may appear and disappear and may drain, ooze, crust or peel easily. The lesions are often painful [3]. Esophagus is only involved in rare cases.
Additional symptoms include:
- Chills
- Fever
- Rapid spread in the amount of sores
- Crusty sores on the scalp (common)
- Achy joints or muscles [4]
- Sores on anus, throat, genitals and other areas
- Raw, painful skin at the site of blister eruption
The problems are chronic in nature.
What Causes Pemphigus vulgaris?
PV is an autoimmune disorder. The immune system, which produces antibodies against invading microorganisms such as bacteria or viruses, start manufacturing antibodies against specific parts of the body itself in sufferers of autoimmune conditions. In PV patients, antibodies are created against a specific protein that binds skin cells together. Consequently, the adhesion between many skin cells gets destroyed and the cells separate from each other. Fluid accumulates within the isolated cells and creates blisters.
The exact etiology for the immune system turning against the body is not known. The possible trigger factors include infection, viruses or other environmental factors [5]. PV may also arise as a side effect of chelating agents, some blood pressure medications and certain other types of drugs.
Pemphigus vulgaris and Diet
Dietary factors have not been explored although it is best to avoid or limit the intake of:
- Spicy and acidic foods
- Foods that contain Tannins (apples, avocadoes etc.)
- Foods that contain Isothiocyanates (broccoli, brussels sprouts etc.)
- Foods that contain Thiols (chives, garlic etc.)
- Foods that contain Phenols (beverages, candy etc.)
- Foods high in phenols (bananas, Black pepper etc.)
Pemphigus vulgaris Risk Factors
This is a non-contagious disease. It is impossible to understand who will suffer from it. However, the susceptibility is increased in middle-aged and elderly people [6].
Pemphigus vulgaris Testing and Diagnosis
Diagnosis can be difficult as PV is rare and because the blisters also arise with various disorders. Detection usually involves:
- Skin and oral examination
- Complete examination of medical history
- Checking for signs of skin peeling (Nikolsky sign)
- Lab tests like skin biopsy, involving microscopic examination of a blister tissue sample
- Blood tests, to detect desmoglein antibodies
Pemphigus vulgaris Differential Diagnosis
Pemphigus vulgaris can be misdiagnosed as bullous pemphigoid. Doctors should distinguish the signs of PV from the symptoms of such disorders.
Pemphigus vulgaris Treatment and Management
Treatment is aimed at reducing the symptoms and preventing complications. Early cure is more effective. Treatment involves:
Medicines
These typically include:
- Corticosteroids
- Biological therapies
- Immunosuppressants
- Antivirals
- Antibiotics
- Antifungal medications
Hospitalization
Treatment during hospital stay involves:
- Fluids (might be intravenous)
- Anesthetic mouth lozenges
- Intravenous feeding
- Therapeutic plasmapheresis
Treatment helps all sores and blisters disappear fully in around 1/3 cases. Others have to take medications on a lower dose for an indefinite period.
Pemphigus vulgaris Complications
Infection of blisters is one of the common complications of PV. In certain cases, the infection can spread fast to the blood (sepsis) and affect the entire body – thus leading to fatal complications.
Other complications include:
- Infection of the skin
- Side effects associated with steroid and immunosuppressant use
- Death from infection (rare)
- Remission (around 70% in sufferers)
Pemphigus vulgaris Prognosis
PV can become chronic with treatment. The side effects may be acute and even disabling. However, treatment generally stops development of blisters and makes them heal. Risk of death is greatly lowered. The outcome has significantly improved since the introduction of steroids [7].
Pemphigus vulgaris Mortality Rate
If left untreated, complications can be life-threatening (due to dehydration). Mortality rate is high with severe infection. Around 1 in 10 PV sufferers die due to severe side effects of treatment. Older patients are at greater risk.
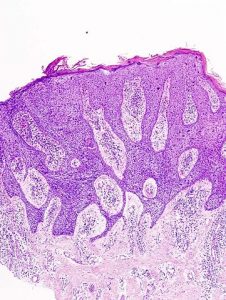
Pemphigus vulgaris Pictures
The images show the sores and blisters arising in PV patients.
Picture 1 – Pemphigus vulgaris
Picture 2 – Pemphigus vulgaris Image
Pemphigus vulgaris Support Groups
Patients may contact the following associations for information and assistance.
International Pemphigus and Pemphigold (IPPF)
1331 Garden Highway, Ste 100
Sacramento CA 95833
United States of America
British Skin Foundation
4 Fitzroy Square
London
W1T 5HQ
Email: [email protected]
Ph: 0207 391 6347/0207 391 6341
The post Pemphigus vulgaris appeared first on Prime Health Channel.
]]>