Keratoconus is an ocular disorder that causes blurred vision, nearsightedness (myopia) and a host of other eye problems in sufferers. Read and inform yourself about this disease, getting enlightened about its possible causes, symptoms, diagnosis, and treatment options.
What is Keratoconus?
Page Contents
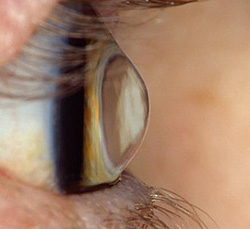
It is a disorder that affects the corneal structure in the eye. The cornea is the transparent layer of tissue that covers the front area of the eye. In individuals affected with this disease, the cornea gradually changes shape and transforms from a normal round size to a conical appearance. This leads to a protrusion (bulging) of the eye, thereby resulting in vision problems.
The disease generally affects both eyes. It typically surfaces during puberty or in the late-teen years of a person.
Keratoconus ICD 9 Code
The ICD 9 Code for this disorder is 371.6.
Keratoconus Incidence
Around 1 out of 2,000 people of the general population are believed to be affected by this eye disorder on an annual basis.
What Causes Keratoconus?
Doctors and medical researchers are still baffled regarding the exact cause of this condition. Certain individuals are supposed to be predisposed to this disease due to heredity. However, an association of this condition with genetic factors has not yet been proved conclusively.
Picture 1 – Keratoconus
The condition is believed to be the result of a defect in collagen, the tissue that renders shape and strength to the cornea.
Certain other possible factors, that are supposed to lead to trauma and degeneration of the ocular tissue, include:
- Rubbing the eye
- Eye allergies
- Wearing contact lenses
Some experts are of the opinion that the disease may be caused due to various factors rather than a single disease.
Keratoconus Symptoms
The disease is characterized by progressive thinning of the cornea as well as its distortion, which occurs over a period of 5 to 10 years. The progression stops after this period.
When the cornea turns cone-shaped, there is an inability of the eye to focus light distinctly on the middle region of the macula (fovea centralis). This leads to significant loss of vision.
In the initial stages of the disease, patients experience mild cases of blurred vision. This cannot be corrected with the aid of glasses. In most cases, however, firm, gas-permeable contact lenses can be used to correct vision to 20/20. Over a period of time, however, sufferers can experience glare, eye halos or other problems with night vision.
Most individuals with this condition suffer from myopia. Distant object appear blurred to them. Over time, this nearsightedness gets worse. Astigmatism arises as the condition worsens.
Certain problems associated with the condition may change over a period of time. These include:
- Problems with night vision
- Heightened sensitivity to glare and bright lights
- Headaches, arising from eyestrain
- Distorted or blurred vision
- Sudden clouding or worsening of vision, resulting from Hydrops (a disorder characterized by rupture of the back of the cornea and its filling with fluid)
Keratoconus Diagnosis
The condition is often diagnosed during adolescence. Certain problems in the eye, as noted by a physician during an ocular exam or as reported to him or her by a patient, can initiate the diagnosis. The typical problems, that doctors use to detect this condition, include:
- Double vision, while looking with only one eye
- Sudden vision change, in only one eye
- Spotting of halos while looking at bright light
- Distortion of objects, both near and far ones
Corneal topography, which renders a map of the corneal curve, is the most exact test for this disease. It involves use of computerized instruments that create three-dimensional map-like images of the cornea.
Some other effective diagnostic techniques for this disorder are:
Eye refraction
It is the standard test used for detecting vision problems. It involves use of a special apparatus that measures the eyes and looks for astigmatism as well as other visual abnormalities. This may involve a measurement done by a computerized refractor which checks the power of focus of the eyes automatically. It may also include Retinoscopy, an ocular exam that makes an assessment of the light reflected by the retina.
A patient may also be asked to look through different lenses to help doctors know which of them helps the person have the sharpest vision. This test also helps physicians understand the extent of vision problems in sufferers.
Pachymetry
This can be used to measure the corneal thickness.
Slit-lamp examination
It can detect the disorder in its later stages. A vertical light beam is projected onto the surface of the eye to let a physician view the corneal shape. The exam may be performed again after eye-drops have been used to dilate the pupils to allow physicians to view the back of the cornea.
Keratometric exam
It involves the use of an apparatus, known as the ‘Keratometer’, which projects a circle of light onto the cornea. The shape of the reflected light lets physicians determine the extent of ocular curvature in affected individuals.
Keratoconus Treatment
The treatment for this disorder depends on its severity and its rate of progression. Contact lenses or eyeglasses are usually enough to address mild to moderate cases of this condition. In case of most sufferers, the cornea is found to stabilize after some years. No serious vision problems arise in affected individuals.
However, around 10-20% of affected people are found to suffer from scarring of the cornea or inability to continue wearing contact lenses.
The standard treatment options for the condition involve:
Contact lenses
These are effective for treating most individuals with this ocular disorder. There are various types of contacts available for curing this condition:
Soft lenses
These are useful in correcting distorted or blurry vision in the initial stages of this eye disease. However, sufferers often need to change these lenses as their corneal shape changes.
Rigid lenses
Also known as “Gas permeable lenses,” these are effective in curing progressive stages of the condition. At first, such lenses may feel uncomfortable to wear. However, most wearers get used to these after a point of time.
Customized lenses
These refer to rigid lenses which are customized to fit a cornea that has changed shape following the development of this disease.
Hybrid lenses
These lenses have a firm center with a softer outer ring to provide added comfort to people who find it hard to tolerate rigid contact lenses.
Piggyback lenses
These are ideal for people who do not like wearing rigid lenses. The name for this type of lens comes from the fact that doctors use a hard contact over a soft lens. In other words, a hard lens is piggybacked over a soft one. Fitting one lens over another requires a lot of precision. Due to this reason, only a doctor who is experienced in performing this technique should be trusted to carry out this job.
Scleral lenses
These are effective in addressing irregular changes in the cornea. Scleral contacts are rested on the white region of the eye (sclera) and vault over the cornea, rather than resting them over the cornea (as is the case with traditional lenses).
Patients who need to wear contact lenses for visual correction should get them fitted by a doctor who has good experience in curing the disorder. Affected individuals also require regular refitting and check-ups. This is due to the fact that a badly-fitting lens can cause further damage to the cornea in case of Keratoconus.
Surgery
A surgical correction is necessary if a patient is unable to wear contact lenses or suffers from poor vision, corneal scarring or extreme corneal thinning despite using the best prescription lenses. A number of surgical procedures are available. The type of operation required depends on the severity of the disorder as well as the location of the bulging cone.
The various operative methods for addressing this disease involve:
Corneal inserts
In this process, two small crescent-shaped plastic segments are inserted into the cornea to support the corneal shape, flatten the cone and improve vision. A local anesthetic is injected into the region around the eye to induce numbness into it. The surgeon uses a laser or precision blade to make a small cut in the cornea. This is immediately followed by the placement of inserts in particular locations, based on the shape of the cornea. The incision is stitched shut and a soft lens is put over the eye to provide it with protection while it heals.
Cornea transplant
Also known as Keratoplasty, this operative technique is used in patients suffering from scarring or extreme thinning of the cornea. In Lamellar keratoplasty, a partial-thickness transplant, only a portion of the corneal surface is replaced. In Penetrating keratoplasty, a total corneal transplant procedure, the full surface of the cornea is replaced.
In Deep Anterior Lamellar Keratoplasty (DALK), the inner corneal layer (known as the endothileum) is kept preserved. The technique helps prevent risks of rejection by endothelial cells, as can occur in a full-thickness transplant.
A new technique, known as collagen cross-linking, is being seen as a promising treatment option for Keratoconus. The procedure involves exposing the cornea to ultraviolet light after applying riboflavin drops onto it. The process strengthens the corneal tissue and prevents its bulging or thinning in later stages. The process is still being tested in the U.S and is likely to be used for general purpose after conclusive results.
Keratoconus Risk Factors
The risk factors for this condition are:
Inherited disorders
A few disorders that are acquired from parents, such as Down Syndrome, can increase the risk of development of this condition.
Certain conditions
A few conditions, such as retinal disorders, connective tissue ailments, asthma or allergies may also make a person susceptible to this disease.
Heredity
Although most sufferers of the disease do not have any family history of Keratoconus, heredity may be a causative factor in certain cases.
Keratoconus Complications
The condition may give rise to the following complications in its sufferers:
Scarring of cornea
Corneal scarring may occur in the advanced stages of the disorder, especially at the site of development of the cone.
Vision problems
Scarring of the cornea may lead to a worsening of visual problems and may need to be cured by corneal transplant operation.
Anxiety
Continuous vision problems arising from this condition can severely affect daily life and activities. This may lead to anxiety in sufferers.
Keratoconus Prevention
In most cases, the condition cannot be prevented. However, certain measures can be adopted to ensure that the disorder does not arise. These include:
Picture 2 – Keratoconus Image
Proper hygiene
Vigorously rubbing the eyes can damage the cornea and consequently give rise to this eye disorder. Although a direct relationship has not yet been established between rubbing and the disorder, it is better to wipe or rub the eyes as gently as possible.
Safe wearing of lenses
It is important to follow instructions while wearing lenses and using them as per the directions of a doctor. The fitting of the lens should be checked on a regular basis to prevent any risk of damage to the eyes. One should strictly avoid using the lenses of someone else.
It is necessary for you to visit an optometrist if your eyesight is rapidly worsening or if you are suffering from irregular ocular curvature (Astigmatism). It is important that you seek medical attention on an immediate basis to safeguard your eyes, two of the most vital sense organs of your body.
References:
Jain A, Paulus YM, Cockerham GC, Kenyon KR. Keratoconus and other noninflammatory corneal thinning disorders. In: Tasman W, Jaeger EA, eds. Duane’s Ophthalmology. 19th ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 2009:chap 16C.
Sugar J, Wadia HP. Keratoconus and other ectasias. In: Yanoff M, Duker JS, eds. Ophthalmology. 3rd ed. St. Louis, Mo: Mosby Elsevier; 2008:chap 4.18.