Periventricular leukomalacia (PVL) is a common form of brain injury affecting many premature infants. Read on to know more about this disease and its potential causes, symptoms, diagnosis and treatment.
Periventricular leukomalacia Definition
Page Contents
- 1 Periventricular leukomalacia Definition
- 2 Periventricular leukomalacia Incidence
- 3 Periventricular leukomalacia Symptoms
- 4 Periventricular leukomalacia Causes
- 5 Periventricular leukomalacia Diagnosis
- 6 Periventricular leukomalacia Differential Diagnosis
- 7 Periventricular leukomalacia Treatment
- 8 Periventricular leukomalacia Prognosis
- 9 Periventricular leukomalacia Prevention
- 10 Periventricular leukomalacia Complications
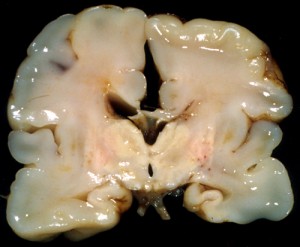
It refers to the softening of the white matter close to the ventricles of the brain that leads to the damage, and sometimes death, of the tissues. Cystic periventricular leukomalacia is a serious type of this disorder involving abnormal formation of cysts near the cerebral region. This is a major condition, which may begin in the fetal stage. It is generally abbreviated as.
Periventricular leukomalacia Incidence
Approximately 4-26% of premature infants are born with a damaged cerebral white matter in neonatal intensive care units. The prevalence of PVL is quite higher according to reports from autopsy studies of premature infants.
Periventricular leukomalacia Symptoms
In most premature infants, PVL is asymptomatic and often goes unidentified. This could be ascribed to mild damage of the white matter, which leads to either display of subtle symptoms or asymptomatic PVL. High degree of white-matter brain injury can, however, produce significant symptoms in older infants. Some of these include:
Picture 1 – Periventricular leukomalacia
- Poor feeding
- Lack of motor skill development
- Acute pulmonary distress
- Cardiac defects
- Abnormally low blood pressure
- Decreased muscle tone in lower extremities
- Irritability
- Increased tone in extensors of the neck
- Temporary cessation of breathing
- Irregular heart rhythm
- Inability to control facial movements such as chewing and speaking
- Seizures
- Involuntary eye movement
- Squint eyes
- Refractive error
- Visual difficulty
Periventricular leukomalacia Causes
Infants who are born before 33 weeks of gestation with a birth weight of less than 1500 g are more susceptible to the condition. PVL is likely to affect neonates with a history of chorioamnionitis, inflammation of the chorion and the amnion surrounding the fetus in some pregnant women. Injury to the white matter of the brain normally begins when the oxygen-laden blood supply to the cerebral ventricles reduces. This ischemic brain injury could result from the followings conditions:
- Hypotension due to depletion of oxygen to the fetus, or cesarean delivery
- Deficiency of oxygen in arterial blood
- Increased acidity in the blood
Another cause of a damaged white matter could be deterioration of the glial cells that surround the neurons of the central nervous system to provide support and insulation between them. The subsequent damage of the white matter adjacent to the ventricles gives rise to cerebral lesions. The other possible causes of PVL, as considered by medical investigators, are:
- Lack of carbon dioxide in the blood
- Placental vascular anastomoses during twin pregnancy
- Profuse vaginal bleeding after the 24th week of pregnancy
- Inflammation of the umbilical cord
- Maternal infection due to cytomegalovirus
- Maternal drug abuse
Periventricular leukomalacia Diagnosis
The identification of symptoms of PVL would be difficult by physicians unless the affected infants mature and reach the developmental milestones such as sitting, walking and crawling. Nevertheless, the possible signs to look for in older children include:
- Tightness of muscles in the limbs
- Contracted legs
- Poor feeding and positioning problems
A few diagnostic procedures that must be carried out to confirm the presence of PVL are as follows:
Imaging studies
Magnetic Resonance Imaging (MRI) scan of the head can reveal regions in the brain damaged by ischemia. The detailed images of the brain obtained signify decreased flow of blood to these areas. In a similar fashion, CT scan of the brain can illustrate the minute details of the periventricular region for any lesions.
Cranial Ultrasound scan
The non-invasive technique can detect the hypoxic-ischemic condition of the cerebral ventricles. The presence of localized lesions in neonates is a warning sign of a possible damage or death of the white matter of the brain.
Periventricular leukomalacia Differential Diagnosis
The medical conditions that need to be considered during diagnosis of PVL are as follows:
- Multicystic encephalomalacia
- Intracerebral hemorrhage
- Subendymal pseudocyst
- Edematous hemorrhagic leukoencephalopathy
- Telentsefalny gliosis
- Diffuse leukomalacia
- Subcortical leukomalacia
- Periventricular hemorrhagic infarction
Periventricular leukomalacia Treatment
There is no treatment measure available at the neonatal level. However, a variety of therapeutic methods are implemented by health specialists for treating conditions that follow PVL. Children with underdeveloped motor skills as well as intellectual disabilities require specialized care and guidance, which is possible through occupational therapy. It includes common interventions like participation in school and social situations, regain of skills, and performing cognitive activities.
As the condition affects vital organs like heart, lung and intestine, the ailing infants must be routinely monitored for any serious complications. The common techniques for correction of neurological deficits in adults cannot be used on the same line for PVL. In fact, some of these treatment methods may negatively affect the health of the newborns. Key research studies have shown the benefits of neuroprotection, a new mechanism that may aid in impeding the loss of neurons due to an injury.
The oxidative stress that constantly builds up during a cerebral ischemia can be counteracted with proper neuroprotective treatments. In this way, the growth of ischemic lesions can be halted or delayed.
Periventricular leukomalacia Prognosis
The degree of white matter damage as well as the severity of the symptoms predicts the prognosis of PVL. Minor injuries may not lead to a fatal outcome. However, those with severe types of brain lesions may develop long-term neurodevelopmental disabilities.
Periventricular leukomalacia Prevention
Prevention of premature birth is perhaps the only solution to reduce the risk of PVL. In order to do this, pregnant women must follow some personal care techniques like:
- Lifestyle management
- Diet and weight control
- Preterm labor medications
- Prolonged bed rest
- Regular medical examination of the growing fetus
- Administration of specific vaccines
- Avoiding stress, smoking as well as intake of illegal drugs and alcohol
The prenatal diagnosis of chorioamnionitis should be followed by prompt treatment of the infection with steroids. Early eradication of the vaginal bacteria can reduce the possibility of PVL. Conditions which impair the maternal-fetal circulation, must be avoided, or treated instantly if detected. Post delivery, the blood pressure of the premature infants needs to be measured mandatorily. Hypotension-affected neonates should be immediately treated with the help of necessary medications required for this condition.
Periventricular leukomalacia Complications
Severe injury of the cerebral white matter could lead to a number of complications. Some of these are:
Picture 2 – Periventricular leukomalacia Image
Spastic diplegia
The condition is marked by increased muscle tone and stiffness in the lower extremities. Affected patients have an abnormal gait and deep tendon reflexes.
Tetraplegia
Damaged white matter may cause partial or total paralysis of all the four limbs.
Cerebral palsy
Acute cerebral ischemic lesions can result in loss of motor function, gait disorders and speech delay.
Epilepsy
Sudden recurrent episodes of convulsions are correlated to PVL.
An early diagnosis of Periventricular leukomalacia is essential as the ensuing complications can be extremely distressing to the infants. Proper maternal and prenatal care limits the incidence of premature births.
References:
http://en.wikipedia.org/wiki/Periventricular_leukomalacia
http://emedicine.medscape.com/article/975728-overview
http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0004493/
http://www.lpch.org/DiseaseHealthInfo/HealthLibrary/neuro/pvl.html