Thrombocytosis is a blood disorder that is marked by headaches, chest pain and loss of consciousness and can even be life-threatening for some sufferers. Read and find out all about this condition, including its primary causes, symptoms, treatment options, prognosis and more.
Thrombocytosis Definition
Page Contents
- 1 Thrombocytosis Definition
- 2 Thrombocytosis ICD9 Code
- 3 Thrombocytosis Types
- 4 Thrombocytosis Incidence
- 5 Thrombocytosis Symptoms
- 6 Thrombocytosis Risk Factors
- 7 Thrombocytosis Causes
- 8 Thrombocytosis Diagnosis
- 9 Thrombocytosis Differential Diagnosis
- 10 Thrombocytosis Treatment
- 11 Thrombocytosis Prognosis
- 12 Thrombocytosis Complications
- 13 Thrombocytosis Pictures
It is a condition characterized by an excessive production of platelets (thromobocytes) in the body, which play a vital role in blood coagulation or clotting. When resulting from an underlying disease, such as an infection, the disease is referred to as “Reactive Thrombocytosis.”
The disorder is also known by the name “Thrombocythemia.”
Thrombocytosis ICD9 Code
The ICD9 Code for this condition is 289.9.
Thrombocytosis Types
The disorder is broadly classified into the following two types:
Primary Thrombocytosis
It is also known by the names Essential Thrombocythemia, Primary Thrombocythemia and Essential Thrombocytosis. It arises as a result of failure in the production and regulation of platelets and is a symptom of various myeloproliferative conditions.
Secondary Thrombocytosis
It is also referred to as Reactive Thrombocytosis. It is generally an exaggerated psychological response to a primary condition, such as an infection. The infection or any other similar trigger factor leads to a release of cytokines that mediate a rise in the production of platelets.
This is often a temporary problem that disappears once the underlying cause is resolved.
Thrombocytosis Incidence
According to an American study, Primary Thrombocytosis has a reported incidence of 2.38 cases in every 100,000 individuals every year. The prevalence of this form of the disorder is around 30 per 100,000 individuals in a population. The incidence of the Secondary form is highest during the first 3 months after birth. Preterm infants are more susceptible to the disease than term infants.
Thrombocytosis Symptoms
The signs and symptoms of Thrombocytosis are based on the type of the disorder that a person is suffering from.
Primary Thrombocytosis Symptoms
Around one-third of all sufferers of this form are asymptomatic at the time of diagnosis. In sufferers, there is an increase in the amount of circulating platelets due to sustained megakaryocyte proliferation. In certain
Secondary/Reactive Thrombocytosis Symptoms
This form rarely gives rise to any symptoms. The signs are more frequently associated to an underlying condition. If the symptoms of Reactive Thrombocytosis arise, they may involve the following:
- Fainting
- Chest pain
- Weakness
- Headache
- Temporary changes in vision
- Lightheadedness or dizziness
- Numbness or tingling sensation in the hands and feet
As Thrombocytosis is not likely to give rise to any problems, patients are usually aware that they have the disorder unless an elevation in the amount of platelets is revealed in a routine blood test. If the blood exam reveals a high platelet count, a doctor would try to find out the underlying cause.
Thrombocytosis Risk Factors
The susceptibility to this disorder may be increased in case of a recently conducted surgery or the presence of a medical disorder such as anemia.
Thrombocytosis Causes
There is no known cause for Primary Thrombocytosis. In some cases, however, it can arise due to a bone marrow condition in which the bone marrow produces excessively high amounts of the cells that manufacture platelets (megakaryocytes) and leads to the release of too many platelets into the bloodstream.
Secondary Thrombocytosis may arise due to a number of health disorders, such as:
- Allergic reactions
- Hemolytic anemia
- Iron deficiency anemia
- Cancer
- Pancreatitis
- Removal of spleen
- Exercise
- Heart attack
- Kidney disorders or Chronic kidney failure
- Infection
- Surgery
- Loss of blood or acute bleeding
- Inflammatory diseases, such as rheumatoid arthritis
The secondary form of the disorder can also be caused due to certain medications which include:
- Epinephrine
- Tretinoin
- Vincristine
Thrombocytosis Diagnosis
The condition may be diagnosed, often accidentally, after one of the following tests is performed:
Physical exam
If a doctor finds an enlargement of spleen or any signs of infection or some other condition during a physical examination, he or she may recommend sufferers to have a CBC (Complete Blood Count) to assess the amount of platelets.
Blood test
A routine blood test reveals a platelet count that is higher than normal.
Blood smear test
In this exam, a small amount of blood is analyzed under a microscope. This helps find out the status of the platelets in sufferers.
As the platelet count can rise on a temporary basis due to a number of diseases, a physician may repeat the blood tests to check whether the amount of platelets remain high over a period of time.
A 150,000 – 450,000 platelet count per microliter of blood is a normal range for platelets. Doctors tend to look for an underlying disorder if the blood count is higher than 500,000.
In the majority of sufferers, the signs and symptoms of a possible underlying disease can help in diagnosis. A physician may also do the following:
- Test for signs of inflammation
- Check the iron level in blood
- Do a biopsy or a bone marrow aspiration to obtain and analyze samples of bone marrow tissue
- Order genetic testing to help find out whether sufferers have a blood disorder or a bone marrow disease
It is essential for doctors to determine whether or not a patient is suffering from the Essential/Primary or the Secondary form of Thrombocytosis.
Thrombocytosis Differential Diagnosis
The differential diagnosis of Thrombocytosis involves telling the symptoms of both of its forms apart from those of other disorders.
Differential Diagnosis of Primary Thrombocytosis
It involves ensuring the signs are not the result of the following disorders:
- Primary myelofibrosis.
- Myelodysplasia with del(5q).
- Primary thrombocytosis (Essential thrombocytosis).
- Chronic myeloid leukaemia.
- Polycythaemia vera (haematocrit is also raised).
- Atypical chronic myeloid leukaemia.
- Chronic myelomonocytic leukaemia.
- Refractory anaemia (with ring sideroblasts related with marked thrombocytosis).
- Myelodysplastic syndrome/Myeloproliferative neoplasm, unclassifiable (MDS/MPN-U).
Differential Diagnosis of Reactive Thrombocytosis
It includes making sure that sufferers are not actually having any of the diseases mentioned below:
- Hyposplenism
- Iron deficiency
- Haemolysis
- Postoperative
- Haemorrhage
- Post-splenectomy.
- Low birthweight/pre-term infants.
- Tissue damage (such as trauma, fracture and burns).
- Cytokine administration (like Thrombopoietin).
- Rebound following myelosuppressive chemotherapy.
- Malignancy (particularly osteosarcoma and soft -tissue sarcoma)
- Renal disorders (like nephritis or nephrotic syndrome).
- Drug therapy (such as those involving adrenaline and corticosteroids).
- Rebound from other causes (such as with iron deficiency anaemia, recovery phase of idiopathic thrombocytopenic purpura (ITP)).
- Infection (common infective causes include urinary tract infections, gastroenteritis, meningitis, infections of the upper and lower respiratory tract, septic arthritis, generalised sepsis and osteomyelitis).
- Inflammation (such as Henoch-Schönlein purpura, Kawasaki disease, inflammatory bowel disease and Rheumatoid arthritis).
Thrombocytosis Treatment
The treatment for Reactive Thrombocytosis is aimed at treating its underlying cause. The elevation in the amount of platelets may not be long-lasting if the cause is a recent injury or an operation that is the cause of significant loss of blood. If the disorder results from an inflammatory disorder or a chronic infection, the amount of platelets may continue to be high until the disease is successfully managed. In the majority of sufferers, the platelet count tends to come back to normal once the underlying cause is resolved.
In some cases, removal of the spleen may result in the persistence of Thrombocytosis for an entire lifetime. In such patients, a physician may prescribe low doses of Aspirin to help prevent cases of blood-clotting or bleeding. However, these problems rarely occur in Reactive Thrombocytosis.
Thrombocytosis Home Remedies
Patients of this disorder can do better and lower the risk of complications associated to this disease by adopting certain lifestyle modification measures. These include:
- Managing any other health problems already present such as diabetes, high cholesterol and high blood pressure
- Giving up, or at least significantly reducing, smoking or use of other tobacco products
- Avoiding passive smoking
- Consulting a doctor or dentist before taking any blood-thinning medicine to manage the symptoms of Thrombocytosis before undergoing any medical procedure. Such drugs can increase the risk of bleeding during such procedures.
- Avoiding use of over-the-counter analgesics (pain-relieving medications) except Acetaminophen (such as Tylenol) and certain cold medicines that may also contain analgesics. It is important to read the labels properly and have a consultation with a qualified doctor before taking any over-the-counter pain-relievers.
Thrombocytosis Prognosis
The outcome of this disorder depends on various factors, such as:
- The form of the condition one is suffering from
- Age of sufferer
- The nature of treatment and how properly it is being conducted
Those with the primary form of the disorder have a 10-year survival rate ranging between 64-80%. This rate may not be much varied from that of the age-matched general population. Death usually occurs from thrombotic complications. In young female patients, doctors can do little to positively affect the pattern of recurrent miscarriage. However, the outcome is significantly non-dangerous for the life and health of affected women.
In case of the secondary form of the disease, the outcome is generally determined by the primary disease.
Thrombocytosis Complications
If an elevation in the amount of platelets is caused by a bone marrow disease in case of Essential rather than Reactive Thrombocytosis, patients may be at risk of developing blood clots. Some of these can be life-threatening.
Primary Thrombocytosis Complications
Some of the typical complications associated to the primary or essential form of this disease include:
- Thrombosis, which can be acute in nature and have life-threatening consequences for sufferers
- Bleeding, generally from the gastrointestinal (GI) tract, which is usually much less acute
- Progression to Acute Myeloid Leukemia, which happens in 0.5-5% of all sufferers
Secondary Thrombocytosis Complications
The complications can develop from the abnormality of platelets but are more often a result of the primary disease.
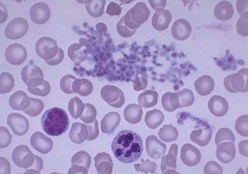
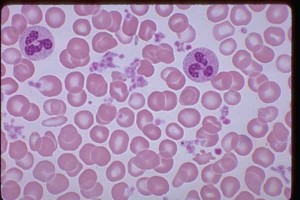
Thrombocytosis Pictures
The following images display the pictures of blood samples of Thrombocytosis sufferers as can be seen under a microscope.
Picture 1 – Thrombocytosis
Picture 2 – Thrombocytosis Image
If you suspect yourself, or any of your family members, to be suffering from Thrombocytosis get a blood test done as early as possible. If a blood examination shows a high platelet count and a Thrombocytosis is confirmed by diagnosis, seek treatment on an early basis. Early detection and treatment can help ensure a better management and faster recovery from this disorder.
References:
http://www.mayoclinic.com/health/thrombocytosis/DS01088
http://en.wikipedia.org/wiki/Thrombocytosis
http://www.patient.co.uk/doctor/Thrombocytosis.htm
http://www.wisegeek.com/what-is-thrombocytosis.htm

I have CKD stage 2 mild and a low Thyroid level right now and this disease is Hereditary on my moms side of the family. I also have GERD, depression, and other diagnosis. Should I be checked for Thrombocytosis?